Can Heart Failure Be Reversed? What You Need to Know About The Role of Lifestyle and Medicine
Heart failure is responsible for the deaths of hundreds of thousands of people around the United States each year. It’s a serious condition and needs to be treated to help curb some of the health issues it causes. Some of the symptoms people often notice that could indicate heart failure include shortness of breath, fatigue and weakness, wheezing, swelling of the belly, fluid buildup, and decreased alertness.
Although it can be a deadly disease and can limit things a person can do in their life, it can be reversed with proper care and attention. Below are some options.
Weight and Heart Failure
As a person’s weight increases, it puts more stress on the heart and can even change the heart’s structure and ability to pump blood. Naturally, this leads to a common question asked by many who have the condition. Can weight loss reverse heart failure? According to doctors and researchers, reducing overall body weight can help to improve symptoms and risks of various illnesses, including heart failure.
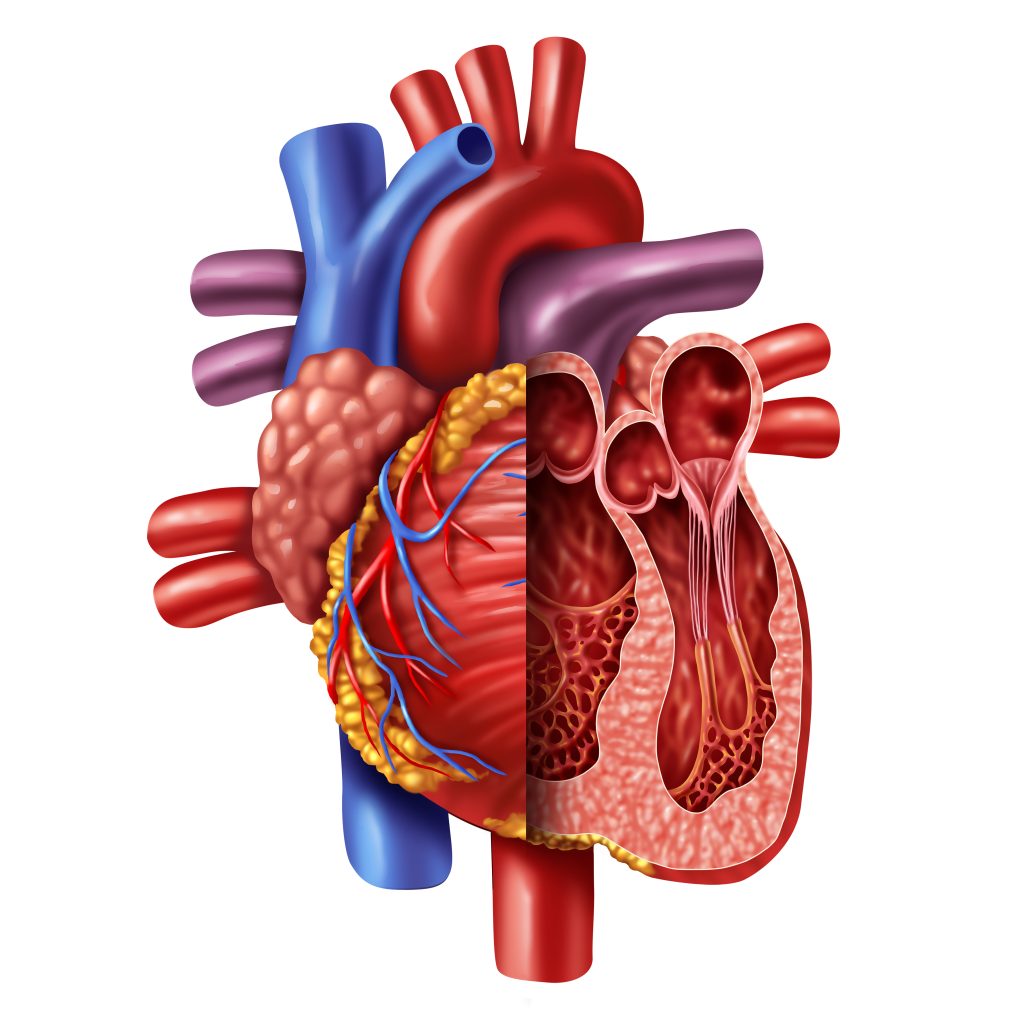
A person who is carrying more weight than is healthy for them will find that over time, it can damage the heart. Because the heart has to pump harder to push blood, the muscle thickens. Those hearts can’t handle the change and may fail. Even relatively small increases in body weight can cause issues with the heart, which is why it’s so important to maintain weight for long-term health.
When someone loses weight, it helps them decrease the thickness of their heart muscle, which could help lower the risk of heart failure.
Heart Failure and Exercise
Can heart failure be reversed with exercise? Research from UT Southwestern Medical Center has found that exercise can reverse damage to sedentary, aging hearts. This could help to prevent the risk of future heart failure. However, it needs to be started in time to be effective. The researchers said that a good exercise routine should be started before the age of 65 when the heart is still capable of remodeling itself. As the heart gets older, it loses plasticity.
They found that exercise not only needs to be started before age 65, but people also need to be doing enough exercise. Two or three days of working out a week don’t produce good results. Researchers said that it needs to be done four to five times per week, typically in 30-minute sessions, not including warm-up and cool-down periods.
Exercise and weight loss can help to reverse heart failure when it’s started early enough. However, losing weight and keeping fit is not always enough.
Can Heart Failure Be Reversed with Medication?
The types of treatment options and medications that may be prescribed to an individual will vary based on the severity of the case. Some of the common medications that are used for treating heart failure include beta blockers, ACE inhibitors, and Aldosterone inhibitors.
Beta-blockers help to block excess adrenaline production, which could cause damage to heart cells. ACE inhibitors are used to relax blood vessels and lower blood pressure. Aldosterone inhibitors block a hormone that causes the body to retain salt and fluid, which promotes heart failure.
Once the medications are added to a patient’s treatment plan, they are also often required to go on a low-sodium diet. This will help the heart grow stronger.
In cases of someone who has extreme heart failure, the options for treatment are often far more invasive. They may include the addition of an implantable heart pump, which will help the heart to continue pumping blood. Another treatment would be heart reconstruction. Sometimes, the only treatment may be a heart transplant.
By incorporating various treatment methods, including weight loss, exercise, and medications, it is possible to reverse some of the damage to the heart, so patients can live a healthier and happier life. This will likely be a problem that continues to follow them. Regardless of what treatment options are recommended, patients will need to continue taking medication. They should also follow up with their cardiologist regularly to monitor their heart health.
Get Help for Your Heart Today
If you have heart failure or you fear that you might be in danger of this condition, it’s important to speak with a medical professional as soon as possible. The doctor can examine you and test your heart health. They can also provide you with medications and ensure you are healthy enough to start an exercise and weight loss plan. The best option is to always seek early treatment.
Cardiovascular Research and Training Institute
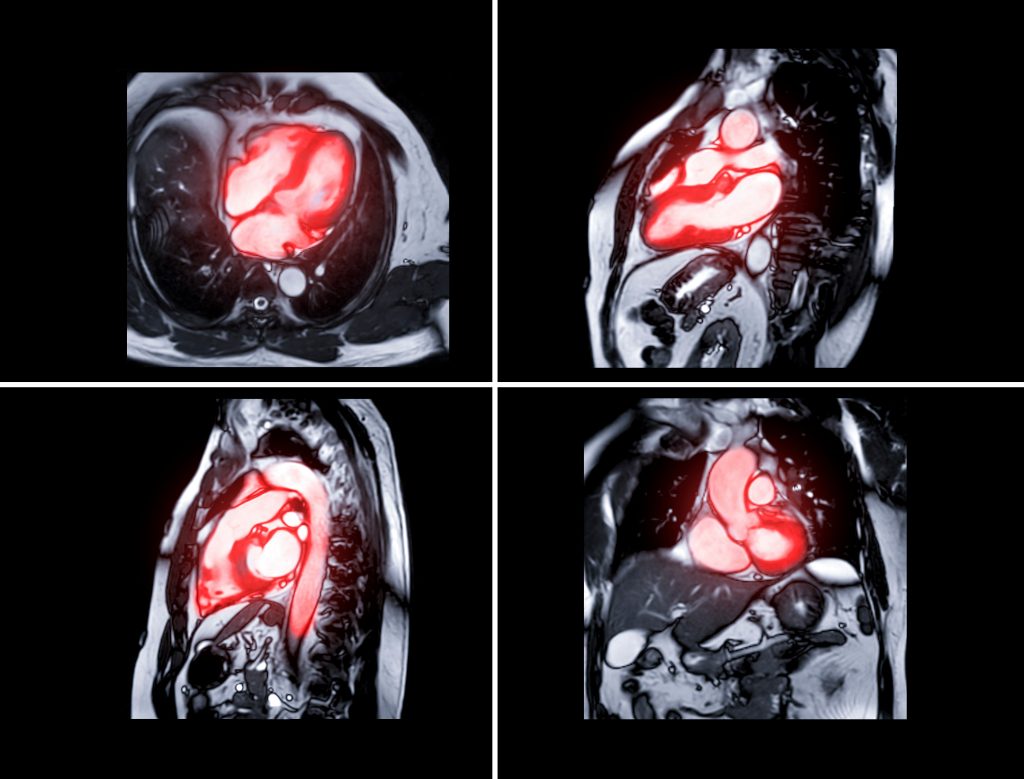
Researchers at the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI) are studying what causes heart muscle to fail and are developing therapeutic strategies to both stop heart failure progression and recover failing hearts. CVRTI Investigators are experts in muscle gene regulation (Franklin), muscle metabolism (Chaudhuri, Drakos), muscle architecture (Hong, Shaw), and treating failing heart muscle (Selzman, Drakos, Dosdall, Hong, Shaw). One therapeutic program involves using surgically implanted left ventricular assist devices (LVADs) to recover failing hearts (Selzman, Drakos). Another involves a promising CVRTI generated gene therapy that rescues failing heart muscle, reverses the damage heart failure does to heart muscle, and improves mortality from heart failure (Dosdall, Hong, Shaw). The therapy is known as cBIN1 gene therapy and is being advanced to clinical trials.