Heart Failure Symptoms, Early Signs, and Stages of Progression
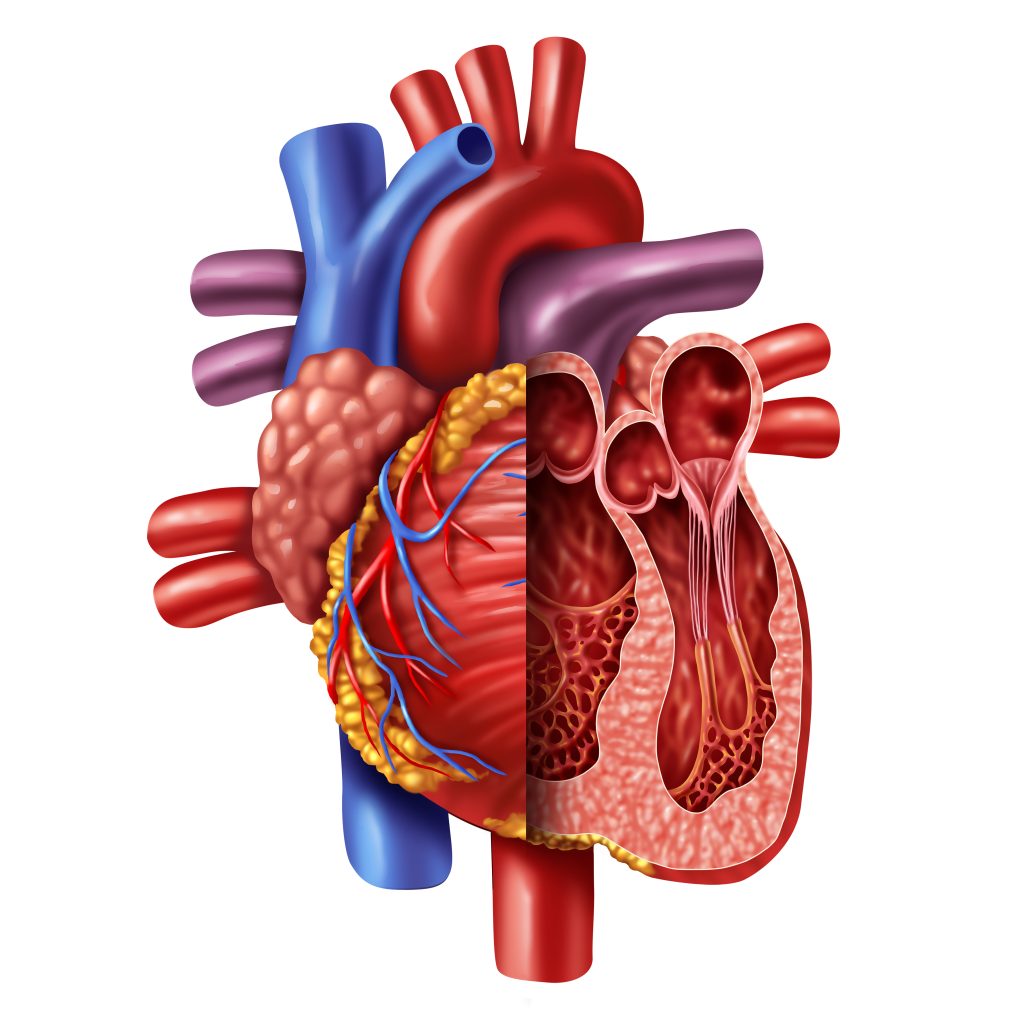
The term “heart failure” may sound as though your heart completely stopped working, but that’s not the case. Heart failure means that the heart is no longer capable of pumping blood as well as it should be. It is a serious long-term condition that worsens over time. When the heart doesn’t pump blood properly, your organs will not be getting the blood needed to perform.
The Early Warning Signs and Symptoms of Heart Failure
Signs and symptoms of heart failure vary in type and severity. Some of the common signs include shortness of breath, swelling in the legs, ankles, and abdomen, and feelings of fatigue when you are active.
People with heart failure might also notice they need to get up more and urinate during the night. They may have irregular heartbeats or a dry, hacking cough. Weight gain can occur, as well. Sometimes the heart failure symptoms are mild or they could vanish entirely. It is important to note that this doesn’t mean that you no longer have heart failure. They may vanish for a time and then return.
For most patients, heart failure will continue to worsen. After a diagnosis, make your doctor aware of any changes to your symptoms.
How Is Heart Failure Diagnosed?
Your doctor will need to know more regarding your medical history, as well as your heart failure symptoms. They may ask whether you have a family history of heart disease or sudden death, whether you smoke or use tobacco, and how much alcohol you drink. They will also want to know what medications you are taking.
They need to know about other health conditions you may have, such as kidney disease, diabetes, high blood pressure, high cholesterol, coronary artery disease, or other heart issues.
The doctor will provide a physical exam to look for early signs of heart failure or other diseases that could have affected your heart muscle. They will often check your ejection fraction, which will let them know how well your ventricles are pumping blood. This can be done relatively easily with noninvasive tests. Normal left ventricular EF is between 53% and 70%.
Other tests that will determine the severity of your heart failure and its cause include various blood tests, cardiac catheterization, chest x-rays, ECGs, MRIs, EKGs, echocardiograms, stress tests, and MUGA scans.
Once the doctor determines the type of heart failure you have and the cause, they can begin treatment. The types of treatment often vary based on the stage.
The Stages of Heart Failure
Below are the stages of heart failure, along with potential treatments used at each stage.
Heart Failure Stage A
When you are at risk but haven’t suffered heart failure yet, you are considered in Stage A. Those who are at this stage can undergo a treatment plan that can help them to reduce their risk of further damage. This includes becoming more active and getting regular exercise, stopping the use of tobacco products, getting treatment for high blood pressure and high cholesterol, and not drinking or using recreational drugs.
Doctors may prescribe angiotensin-converting enzyme inhibitors or an angiotensin II receptor blocker for those who have high blood pressure, diabetes, coronary artery disease, or other cardiac issues. Beta-blockers might also be prescribed for those with high blood pressure.
Heart Failure Stage B
This is also considered pre-heart failure. The doctor has found that you have systolic left ventricular dysfunction, although you don’t have symptoms of heart failure.
In addition to the Stage A treatments, the doctor might also prescribe an aldosterone antagonist if you have diabetes or have had a heart attack and have an ejection fraction of 35% or less. In some cases, surgery may be required.
Heart Failure Stage C
Those with Stage C heart failure currently or previously had some or all of the signs and symptoms mentioned above. The Stage A and B treatments are still employed along with medications that can slow the heart rate if it’s above 70 bpm and the heart failure symptoms remain.
If Heart Failure Symptoms Continue
Diuretic pills may be used if heart failure symptoms continue, and sodium will be restricted. At this stage, patients must track their weight daily and let the doctor know if there is a change of more than four pounds. Fluid restriction could be required in some patients. The use of a biventricular pacemaker could also be required as a means of cardiac resynchronization therapy.
Heart Failure Stage D
At this point, the patient has advanced heart failure symptoms that will not get better with treatment. It is the final stage of heart failure. At this point, in addition to the treatments used for the earlier stages, more advanced treatments are needed. This may include ventricular assist devices, a heart transplant, heart surgery, or hospice care.
Patient outcomes will vary. Those who have heart failure or who are worried they are at risk should speak with their doctor as soon as possible. Getting a diagnosis and treatment as early as possible can make a difference.
Cardiovascular Research and Training Institute
Researchers at the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI) are studying what causes heart muscle to fail and are developing therapeutic strategies to both stop heart failure progression and recover failing hearts.
CVRTI Investigators are experts in muscle gene regulation (Franklin), muscle metabolism (Chaudhuri, Drakos), muscle architecture (Hong, Shaw), and treating failing heart muscle (Selzman, Drakos, Dosdall, Hong, Shaw). One therapeutic program involves using surgically implanted left ventricular assist devices (LVADs) to recover failing hearts (Selzman, Drakos).
Another involves a promising CVRTI generated gene therapy that rescues failing heart muscle, reveres the damage heart failure does to heart muscle, and improves mortality from heart failure (Dosdall, Hong, Shaw). The therapy is known as cBIN1 gene therapy and is being advanced to clinical trials.