What is an EKG Test and How is it Used in Heart Medicine
What Is An Electrocardiogram? (EKG)
An electrocardiogram, also known as an EKG or ECG, is a safe, non-invasive test that helps your doctor monitor for heart disease. The test monitors the electrical activity of your heart through electrode-stickers placed on the skin of your arms, legs, and chest.
EKGs Are Used by Doctors to Diagnose or Monitor Several Heart-Related Issues:
- Irregular heart rhythm
- Inadequate or poor blood flow to the heart muscle known as ischemia
- A heart attack
- The thickness of the heart muscle
- Electrolyte—potassium, calcium—abnormalities in the blood
How Do You Prepare for an Electrocardiogram?
An electrocardiogram is non-invasive, but there are a few things you should do the day of that will make it go smoothly. Your doctor will likely give you a prep list, but here are the basics.
- Ensure your skin is clean and there’s no soap, lotion, or skin creams on you. The residue of those products can make it difficult for the electrodes to stick to your skin correctly.
- Wear a loose or easily removed shirt for accessibility to your chest area. (Some testing centers will supply you with a hospital-style gown, but others allow you to remain in your street clothing.) Short sleeves are also recommended as electrodes need to be placed on your arms as well.
- Ladies should avoid full-length clothes. Electrodes need to be placed on your legs.
- Consider wearing shorts to make it easier to place electrodes.
How is an Electrocardiogram Administered?
With adhesive pads, ten electrodes are attached to your chest, arms, and legs. You will then lie flat, and a computer measures your heart’s electrical impulses and graphs them onto the graph paper. The technician who attached the electrodes will monitor the test and remove the electrodes when finished.
The electrocardiogram takes approximately ten minutes for the attachment of electrodes and test completion. The information-gathering portion of the test is only a few seconds in length. Depending on your symptoms, your doctor might order this resting EKG, or they might order one that is completed while you exercise. Either way, your results will be added to your medical record to be used as a comparison with future tests.
Types of EKG Tests
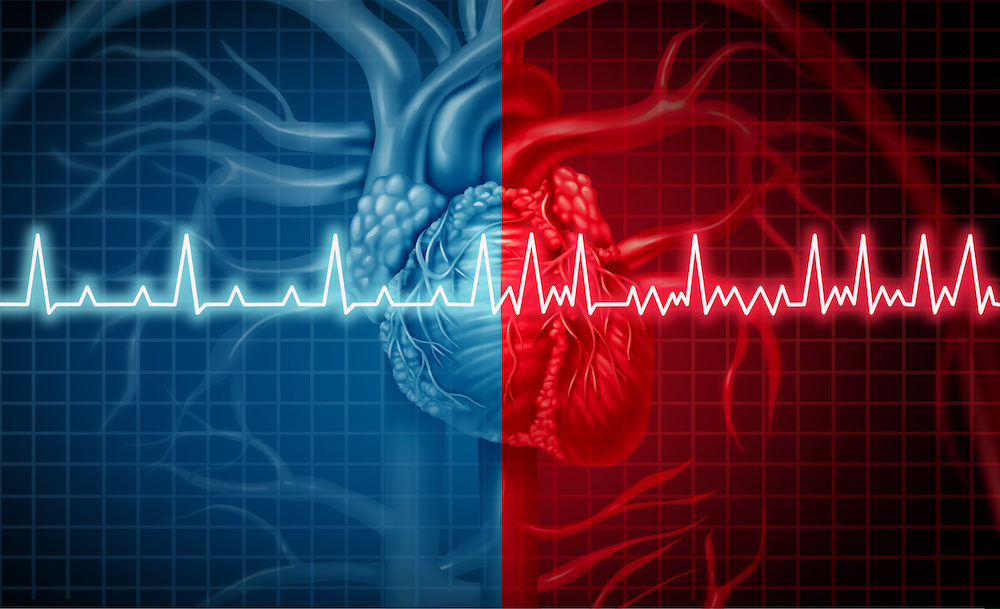
On occasion, your doctor may need more information than a standard EKG provides. In that circumstance, the doctor may order one of two other kinds of electrocardiograms. Both are painless and are administered similarly to a regular EKG.
Event Monitor
An event monitor is like an EKG with one addition. It has a button to be pushed when you notice symptoms. When the button is pressed, the event monitor begins recording and continues to do so for a few minutes. These electrocardiogram machines are typically small adhesive patches that are worn for a few weeks or longer, depending on the symptoms and the data the doctor needs.
Holter Monitor
A Holter monitor is portable and takes readings for a day or two for the entire 24-hour period. With a Holter monitor, you wear the device home and complete your regular daily tasks (except showering) for the duration of the test. This test helps diagnose abnormal heart rhythms, decreased blood flow to the heart muscle, and the cause of palpitations.
Conclusion on EKG Tests & Their Uses in Monitoring Heart Disease
An electrocardiogram, also known as an EKG or ECG, is a simple, safe, non-invasive way for doctors to monitor a patient’s heart. A technician administers the test and reports the results to the doctor. Results are placed in the patient’s medical record for later comparison with other tests. The test itself takes approximately 10 minutes, but the computer records only a few seconds of that. Monitoring such as Holter and Event monitors are simpler forms of ECGs that record the electrical signals over longer periods of time.
Cardiovascular Research and Training Institute
Researchers at the CVRTI use EKG technology to study the electrical activity of every aspect of cardiac disease from the cell to the bedside. We have Investigators who place microscopic electrodes in isolated cells to measure the electrical currents that contribute to the EKG and our physician scientists have developed highly sophisticated EKGs that can be used on patients, extending the diagnostic information gained from heart monitoring. Over its fifty-year history, the CVRTI has been instrumental in developing advanced techniques to measure electrical rhythm, which are now used in hospitals all over the world. At present, our researchers are now developing new therapeutic solutions for patients suffer from electrical disturbances of the heart.


 The Drakos Laboratory, headed by Stavros Drakos, MD, PhD, focuses on understanding the metabolic and molecular profile of the failing and recovered heart and utilizes biological information derived from studies in humans, small, and large animal HF models to understand, predict and manipulate myocardial recovery. Original work generated by the Drakos research team in the laboratory and in the clinical arena led to the founding and establishment of the award winning multidisciplinary Utah Cardiac Recovery Program (UCAR). Link to lab summary page on CVRTI
The Drakos Laboratory, headed by Stavros Drakos, MD, PhD, focuses on understanding the metabolic and molecular profile of the failing and recovered heart and utilizes biological information derived from studies in humans, small, and large animal HF models to understand, predict and manipulate myocardial recovery. Original work generated by the Drakos research team in the laboratory and in the clinical arena led to the founding and establishment of the award winning multidisciplinary Utah Cardiac Recovery Program (UCAR). Link to lab summary page on CVRTI 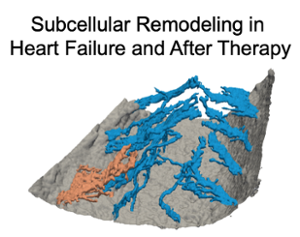 The Sachse Laboratory, headed by Frank Sachse, PhD, provides insights into structural and functional remodeling in diseased hearts and mechanisms of cardiac recovery after clinical therapy. They also develop optical approaches to support pediatric heart surgery and interventional cardiology.
The Sachse Laboratory, headed by Frank Sachse, PhD, provides insights into structural and functional remodeling in diseased hearts and mechanisms of cardiac recovery after clinical therapy. They also develop optical approaches to support pediatric heart surgery and interventional cardiology.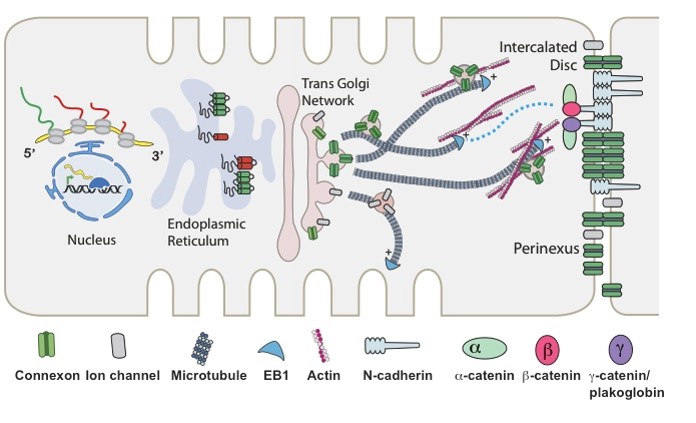 The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI
The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI 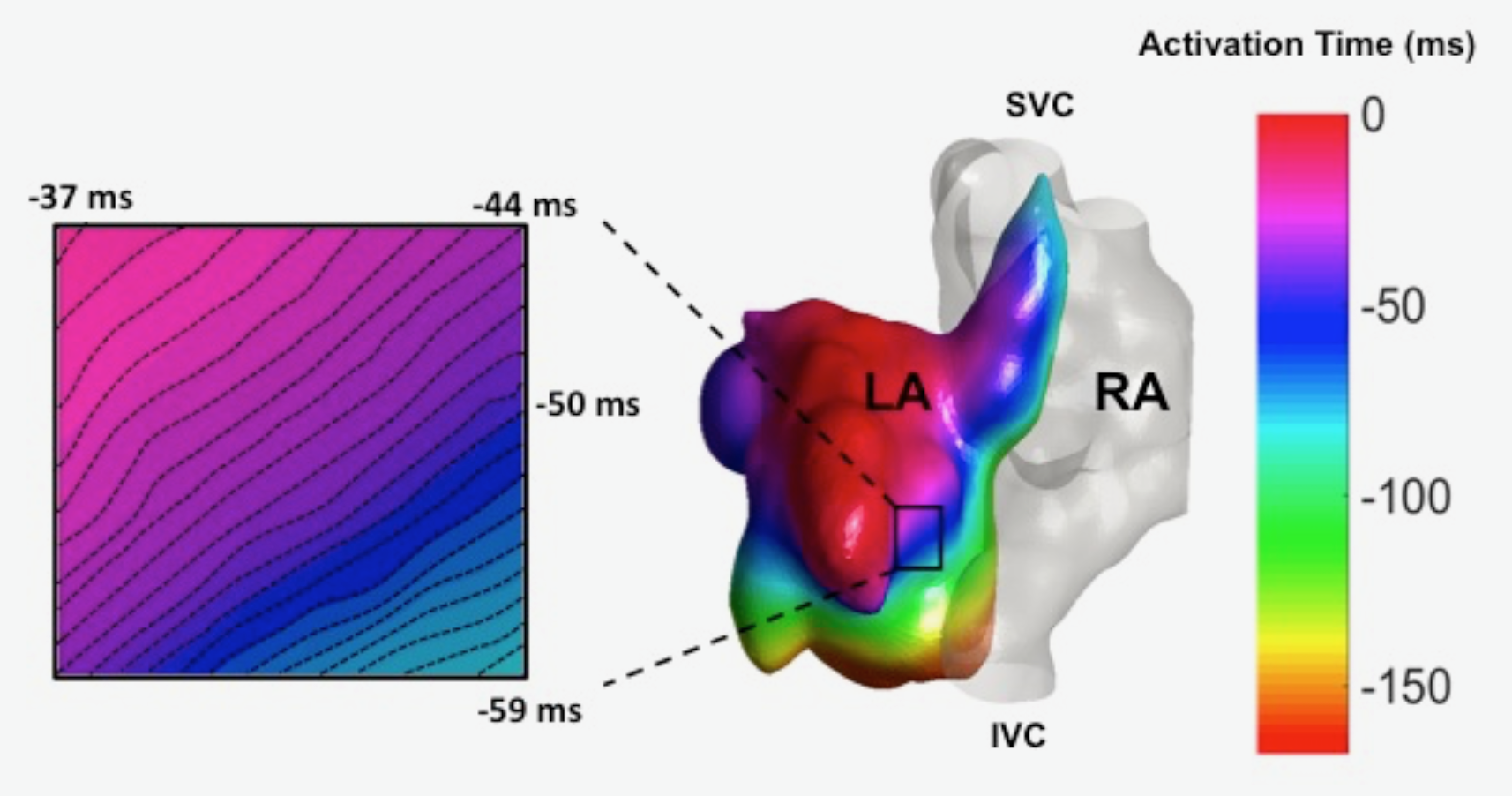 The Ranjan Laboratory, headed by Ravi Ranjan, MD, PhD, focuses on developing a better understanding of arrhythmia mechanisms and optimizing the ablation procedure. The lab is using a combination of high density electrical mapping and imaging in an animal model combined with computational modeling to develop a better understanding of arrhythmia mechanisms. To optimize the ablation procedure, the team uses MRI to quantify tissue changes including reversible edema over time for different energy sources and ablation parameters to develop the optimal ablation technique. Link to lab summary page on CVRTI
The Ranjan Laboratory, headed by Ravi Ranjan, MD, PhD, focuses on developing a better understanding of arrhythmia mechanisms and optimizing the ablation procedure. The lab is using a combination of high density electrical mapping and imaging in an animal model combined with computational modeling to develop a better understanding of arrhythmia mechanisms. To optimize the ablation procedure, the team uses MRI to quantify tissue changes including reversible edema over time for different energy sources and ablation parameters to develop the optimal ablation technique. Link to lab summary page on CVRTI