Effects of Epigenetics in Cardiovascular Disease & Research
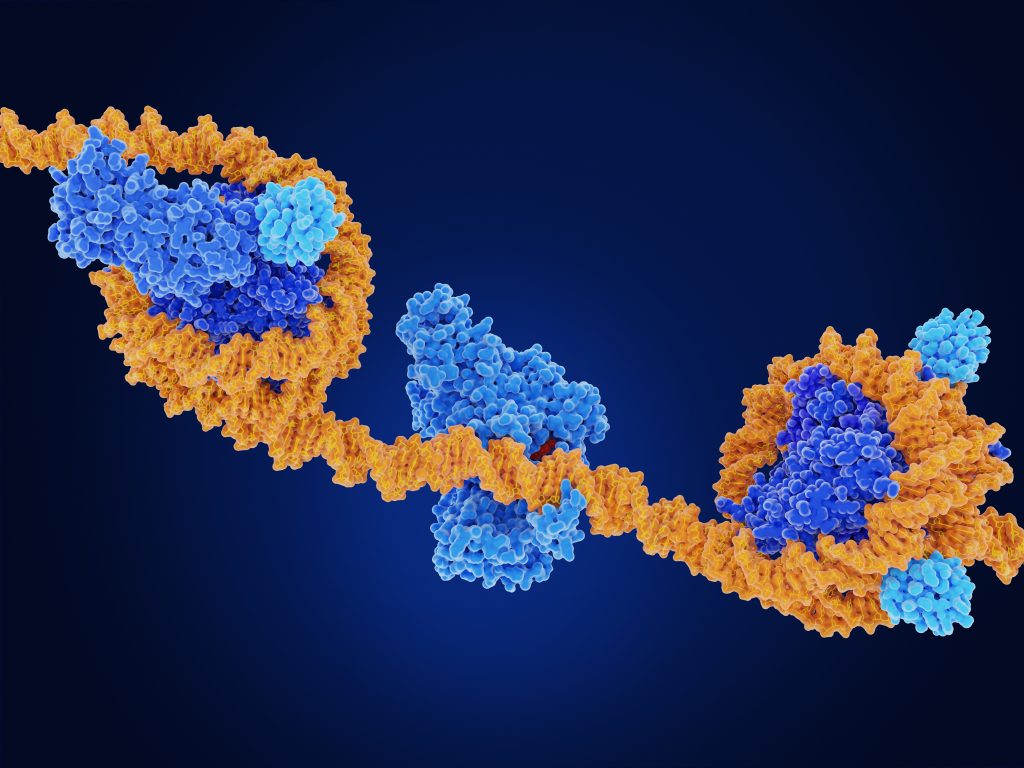
In biology, epigenetics is the study of heritable changes that do not involve alterations in the DNA sequence. The Greek prefix ‘epi’ means over, outside of, or around. Thus, its definition is the feature of the genetic code that exists or develops in addition to traditional genetic inheritance.
Epigenetics is, in essence, the study of how things like lifestyle choices and the environment can cause changes that affect the way your genes work, including what diseases you become predisposed to. Most epigenetic changes are reversible; however, their effects can worsen or cause diseases that are not.
Epigenetics has emerged as a powerful tool to aid in the therapeutic treatment of cardiovascular disease by looking closely at the epigenetics of cardiovascular patients and customizing treatment plans based on someone’s unique epigenetic factors.
Studies That Link Epigenetics and Cardiovascular Disease
Epigenetics was initially studied in patients with cardiovascular disease to better understand their prominent role in inflammation and vascular involvement. These studies in cardiovascular patients showed a significant number of certain epigenetic modifications affecting the development and progression of cardiovascular disease.
In the case of cardiovascular hypertrophy, epigenetics studies found that cardiac hypertrophy is linked with histone acetylation, implicating both histone acetyltransferases (HATs) and histone deacetylases (HDACs).
Cardiac Arrhythmias
Epigenetics has also been studied in afflictions like cardiac arrhythmias. Atrial fibrillation is one of the most common heart arrhythmias, particularly in older patients, and can be deadly. In a study done on its role in atrial fibrillation, transgenic mice were programmed to develop cardiac hypertrophy, and then treated with an epigenetic approach, “Liu and colleagues showed that an injection of a specific HDAC inhibitor reverses atrial fibrosis and diminishes atrial fibrillation vulnerability following an electrical stimulation.” (1)
Among miRNAs that have been widely studied in experimental environments, miR-1 was found to be essential in normal electrophysiological conduction. When miR-1 was deleted in rodents, the rate of sudden death was much higher. This points to the idea that the miR-1 subtype of miRNAs is essential to healthy cardiac rhythms and lowering levels of miR-1 could signal an oncoming arrhythmia. Epigenetic interventions can more effectively return the heart back to a normal state when combined with traditional methods.
Atherosclerosis
In atherosclerosis (hardening of the arteries or artery disease), epigenetic studies reveal some key factors to recognize developing atherosclerosis, sometimes before the patient even feels symptoms. DNA methylation, miRNAs, and epigenetic mechanisms have all been described in atherosclerosis. Two studies were done that show coexisting DNA methylation alongside atherosclerotic lesions in rodents. Interestingly, it was observed that DNA methylation could often be detected in animals far before the anatomical presentation of the disease itself. In short – DNA methylation testing could stand as a powerful screening tool to determine the early stages of atherosclerosis.
Diabetes and Cardiovascular Disease
In studying the relationship between diabetes and cardiovascular disease, epigenetics can be used to demonstrate the effect of untreated or poorly treated diabetes on worsening heart disease. In a study conducted and published by Louisa Villeneuve and colleagues, they found connections between diabetes and the inflammatory epigenetic reactions that can be caused by high glucose.
This study found that the occurrence of inflammatory genes in vascular cells that were exposed to high glucose for extended periods was increased. (2) Conversely, they found that histone H3 (specifically, H3K9me3), which is known to guard the body against the biochemical effects of diabetic inflammation, were decreased in environments in which they had to succumb to high glucose. The finding shows that uncontrolled glucose levels (usually caused by uncontrolled or poorly treated diabetes) can simultaneously cause inflammatory reactions while hindering the effectiveness of key histones like H3K9me3.
In all studies that have been completed, one thing was clear. Epigenetic changes are a clear indicator that can tell us important information about a patient’s ongoing cardiovascular disease or likelihood of developing impending cardiovascular disease.
Conclusion on Epigenetics and Cardiovascular Research
Epigenetics are genetic changes that happen in reaction to external factors. These external factors are usually caused by environmental or lifestyle exposures. Epigenetic changes can be important ‘warning signs that a disease is worsening or about to occur. Furthermore, by studying epigenetics in relation to heart disease, we can get a better idea of what prevention and intervention tactics should be taken.
Epigenetic factors and expressions are somewhat unique and can vary from patient to patient, but overall, there are quantifiable patterns of what role epigenetics plays in cardiovascular disease. Studying these micro-changes can make a big difference in preserving the quality of life in patients with cardiovascular disease and aid in early detection of patients with epigenetic risk factors for the disease.
Cardiovascular Research and Training Institute
Researchers at the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI) are focused on understanding the epigenetic factors that alter transcription and thereby cardiac physiology during the development of arrhythmias, cardiac hypertrophy, and heart failure. Specifically, research at CVRTI has centered on understanding the role of lysine methyltransferases in modifying histones within the nucleosome, characteriz ing specific histone modifications that are differentially regulated during disease, and identifying the role of transcription factors in pathological remodeling and reverse remodeling . These studies have utilized zebrafish , mouse models and human induced pluripotent stem cells as transgenic models of disease to further our understanding of these key processes. By incorporating cutting-edge technology with novel animal models of disease, the epigenetics research at CVRTI is making significant contributions not only to basic science, by elucidating the fundamental basis of gene expression and transcriptional regulation in the cardiomyocyte, but also to the clinical realm by identifying key regulators of cardiac pathophysiology that may also protect the heart from ischemic injury or heart failure.