Top Heart Failure Causes

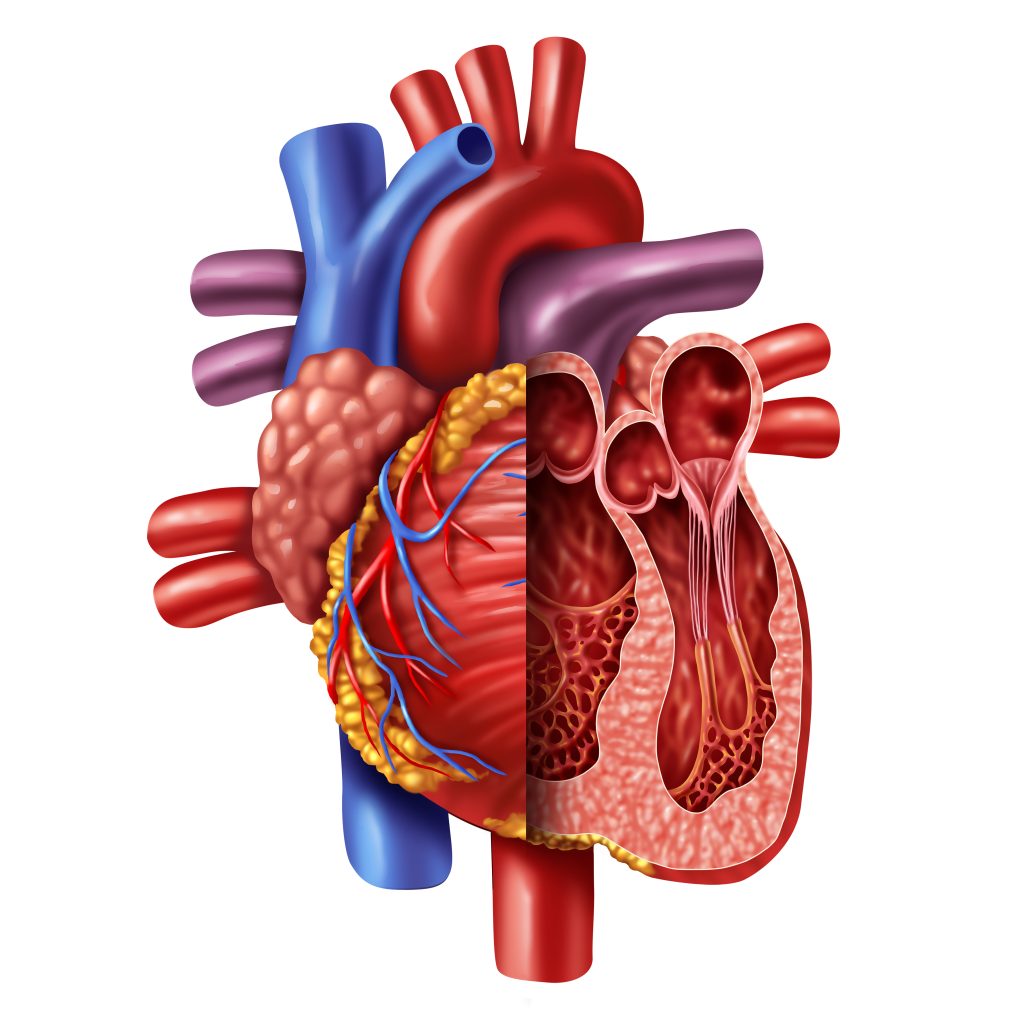
What is Coronary Heart Failure?
Heart failure is a condition that kills hundreds of thousands of people in the United States annually. People often put their hearts at risk without fully understanding just how much damage they can cause. Being overweight, eating unhealthy foods, not being physically active, and smoking could all promote heart failure. Additionally, other health issues can create more wear on the heart, which can lead to a higher risk.
The Effects of Coronary Artery Disease on Heart Failure
Coronary artery disease tends to cause high blood pressure, as the arteries become more and more clogged with cholesterol and fatty deposits. High blood pressure could lead to heart failure over time. If someone has suffered a heart attack in the past, it can weaken and damage the heart tissue, which reduces its ability to pump blood. This can also lead to an increased risk of heart failure.
What Can Cause a Weak Heart
Abnormal heart valves and heart defects at birth can cause a weakened heart, as can heart muscle diseases and inflammation. The hearts of people who suffer from severe lung disease must work hard to get oxygen to the rest of the body, which causes a lot of wear. Over time, this can lead to heart disease. Some of the other potential causes of failure and heart disease include sleep apnea, diabetes, abnormal heart rhythm, severe anemia, and hyperthyroidism.
As you can see, there’s no single factor that will cause heart disease. It can stem from a range of conditions and lifestyle choices.
Types of Heart Failure
When discussing this condition, it is important to understand that there are not only multiple causes, but also multiple types of heart failure.
Left Ventricular
The left ventricle of the heart pumps blood to the rest of the body and is responsible for most of the pumping power. It is larger than the other chambers of the heart.
There are two types of left ventricular heart failure
First, there is a systolic failure, which means the left ventricle is no longer capable of contracting properly, so the blood can’t be pushed through the body. Second is a diastolic failure. This means that the left ventricle cannot relax normally because the muscle has stiffened.
Right Ventricular
The right ventricle pumps blood from the heart to the lungs, so it can be filled with oxygen. This type of failure usually happens because there is a left ventricular failure. Fluid pressure is pushed back through the lungs, damaging the right ventricle. This may cause swelling in the legs and ankles, as well as the abdomen.
Congestive Heart Failure
Congestive heart failure requires that patients get medical attention right away. In these cases, the blood is pumping out of the heart slowly, and when it returns, it begins to back up and cause congestion in the body, which causes swelling. The fluid could also collect in the lungs, which can make breathing difficult, especially if the patient is lying down. This is known as pulmonary edema, and it could cause respiratory distress when not treated promptly.
Stages of Heart Failure
There are four stages of heart failure—A, B, C, and D.
Stage A
Someone who is at Stage A is considered at high risk for heart failure, but they haven’t yet developed structural heart disease or symptoms associated with heart failure.
Stage B
At Stage B, the person has identifiable structural heart disease or cardiomyopathy, but they still don’t have the usual symptoms associated with heart failure.
Stage C
When someone reaches Stage C, they have structural heart disease and will likely have prior or current heart failure symptoms.
Stage D
Stage D involves refractory heart failure and requires medical intervention and treatment for the patient.
Ideally, a patient will already be speaking with their cardiologist and taking steps to prevent further damage to their body. Treatments vary for the different stages, and it’s always best to follow the advice of the doctor.
How Is Heart Failure Diagnosed?
Doctors can administer a wide range of tests to determine whether someone has heart failure. This includes blood tests, as well as electrocardiograms (ECGs). The ECG will record the electrical activity in the heart to look for any issues. Some of the other options include echocardiograms, chest x-rays, ejection fraction, stress tests, CT scans of the heart, cardiac MRIs, coronary angiograms, and myocardial biopsies.
The test a patient is given will depend on their current condition and what the doctor feels will provide the best results. The doctors will also discuss various methods of treatment if heart failure or other issues are discovered.
Cardiovascular Research and Training Institute
Researchers at the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI) are studying what causes heart muscle to fail and are developing therapeutic strategies to both stop heart failure progression and recover failing hearts. CVRTI Investigators are experts in muscle gene regulation (Franklin), muscle metabolism (Chaudhuri, Drakos), muscle architecture (Hong, Shaw), diagnosing (Hong, Shaw) and failing heart muscle treatment (Selzman, Drakos, Dosdall, Hong, Shaw). One therapeutic program involves using surgically implanted left ventricular assist devices (LVADs) to recover failing hearts (Selzman, Drakos). Another involves a promising CVRTI generated gene therapy that rescues failing heart muscle, reverses the damage heart failure does to heart muscle, and improves mortality from heart failure (Dosdall, Hong, Shaw). The therapy is known as cBIN1 gene therapy and is being advanced to clinical trials.