Symptoms and Causes of Cardiac Arrhythmia: How Can It Affect Your Body?
Cardiac arrhythmia is a medical term used to denote an irregular heartbeat or heart rhythm. Electrical signals in the body help ensure a normal, steady heartbeat. Heart arrhythmia occurs when those electrical signals are not working properly. Sometimes, heart arrhythmias can be harmless, but they may indicate serious and potentially life-threatening issues.
Types of Heart Arrhythmias
Arrhythmia or irregular heart rhythm can cause one of three issues. The heart might beat irregularly. It may also beat too fast (tachycardia) or too slow (bradycardia). Any of these issues could affect your body.
Keep in mind that it’s normal for a person’s heart rate to change during various activities. The heart rate slows while sleeping and speeds up during exercise, for example. The problems come when the resting heartbeat is too fast, slow, or erratic.
Arrhythmia Type 1: Tachycardia
Tachycardia refers to a resting heart rate that is higher than 100 beats per minute. Several types of tachycardia exist, as noted below.
Atrial fibrillation causes a chaotic, rapid, and uncoordinated heart rate, which is associated with stroke. Atrial flutter is another type of tachycardia. The beats are more organized than atrial fibrillation or afib, but this is also linked to stroke.
Supraventricular tachycardia refers to heart arrhythmia that begins above the ventricles and causes palpitations that start and end abruptly.
Ventricular fibrillation causes the ventricles to quiver rather than contract and pump the blood to the rest of the body. This is potentially a deadly condition if the normal heart rhythm is not restored in minutes. Those who have ventricular fibrillation generally have heart disease or have suffered serious trauma to the heart.
Ventricular tachycardia is a regular but rapid heartbeat that doesn’t allow the ventricles to fill with blood. The heart can’t pump blood to the rest of the body. If someone has an otherwise healthy heart, this may not cause serious problems. However, this is a medical emergency for those who have heart issues.
Arrhythmia Type 2: Bradycardia
Those who have a heart rate that is below 60 beats per minute could have bradycardia. However, a low resting heart rate isn’t always a sign of an issue. People in top physical condition may have a slow heart rate simply because their body doesn’t need to work as hard to pump blood.
However, those who have a slow heartbeat and the heart isn’t pumping enough blood could have one of two types of bradycardia—sick sinus syndrome or conduction block.
The sinus node sets the pace for the heart. If it is not working properly, the heart may beat too slowly for a time and then alternate to beating too fast. This tends to be a more common problem with older adults. Conduction block occurs when the electrical pathways in the heart are blocked. It can cause the heart beats to slow or stop.
Arrhythmia Type 3: Premature Heartbeats
These are essentially extra beats of your heart. They may follow a pattern and alternate with the normal heartbeat, or they could be erratic. When this occurs, it may feel as though your heart literally “skipped a beat”.
Most of the time, premature heartbeats will not be a concern unless you have a more serious health condition.
Those who have heart disease, for example, may find that a premature heartbeat creates a longer-lasting arrhythmia. People who have frequent premature beats that last for several years may find that it leads to a weakened heart.
Common Symptoms of Heart Arrhythmia
In some cases, you may not notice any signs or symptoms of heart arrhythmia. It might only be detected when a doctor examines you for a different medical health issue. Others, however, will notice some of the more common arrhythmia symptoms noted below.
These include a fluttering feeling in the chest, shortness of breath, or chest pain. You might also notice an irregular heartbeat – a racing heartbeat or a slow heartbeat. Some of the other arrhythmia symptoms that might be present include fatigue, anxiety, dizziness, sweating, fainting, or near fainting.
What Causes Heart Arrhythmia?
Heart arrhythmia could be caused by any number of health issues including coronary artery disease, high blood pressure, cardiomyopathy, or valve disorders. Some may have irritable tissue in the heart, which could come from genetic issues or acquired causes.
Those who have had a heart attack before and who have a damaged heart may develop heart arrhythmia. During the healing process after undergoing heart surgery, the heart may be arrhythmic. Even electrolyte imbalances in the blood could create arrhythmia for a time.
Premature heartbeats can be caused by stimulants like caffeine and nicotine, strenuous exercise, and stress.
Consult with a Doctor About Your Heart Health
When you feel as though your heart is beating too fast or too slow or if you experience any heart arrhythmia symptoms, contact a doctor and make an appointment for medical health treatment. Immediate medical attention should be sought if the change in your heartbeat is accompanied by lightheadedness, weakness, shortness of breath, or chest pain/discomfort.
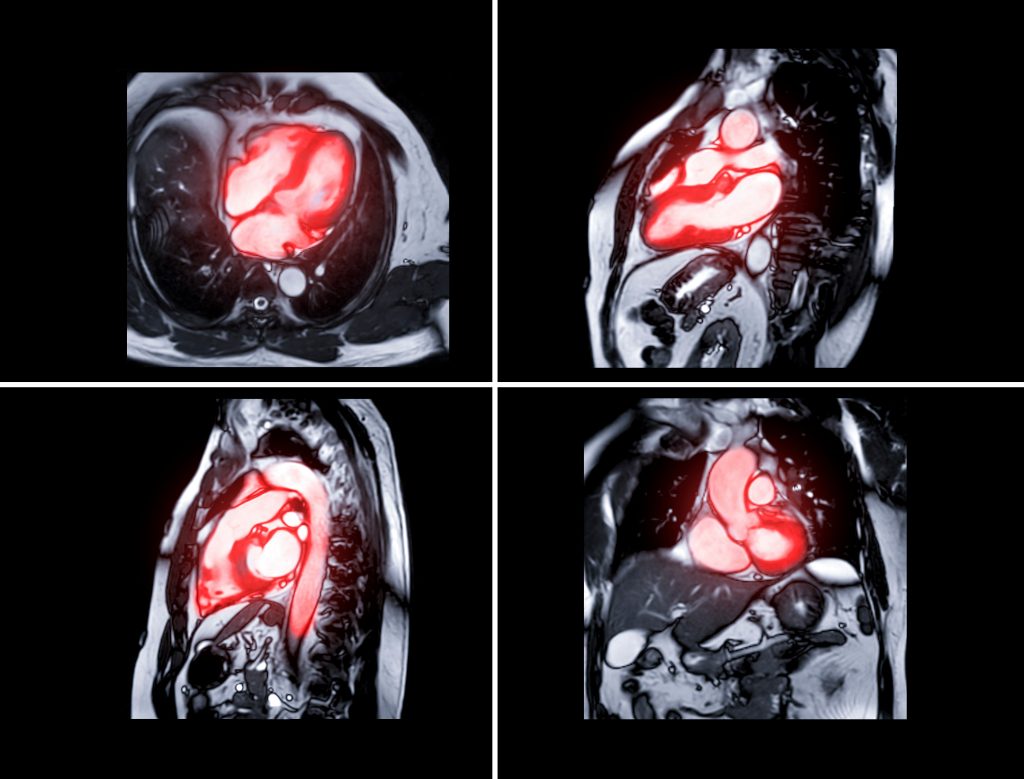
Cardiovascular Research and Training Institute
Researchers at the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI) are studying what can impact the heart’s electrical patterns and how to best diagnose, maintain, and treat cardiac arrhythmias or irregular heart rhythms. The CVRTI is committed to better understanding how to maintain a healthy heart and improve heart health outcomes. CVRTI is famous because, thirty years ago, its Investigators discovered the molecular basis of the most prominent genetically acquired arrhythmia syndrome (“Long QT Syndrome”) and identified how common medicines can result in these highly dangerous arrhythmias. Now, Investigators are studying the mechanisms underlying afib or atrial fibrillation and ablation techniques with the goal of improving ablation outcomes (Ranjan). They are also studying techniques to prevent and terminate life threatening arrhythmias or irregular heartbeats without the need for shocking the heart (Dosdall, Shaw). The genetic and metabolic basis for some of these arrhythmias is also being investigated (Aromolaran, Palatinus, Tristani). Research at CVRTI is changing irregular heartbeat or cardiac arrhythmia patients. Contact CVRTI to learn more about ongoing medical health research and treatment for cardiac arrhythmia.