Cardiogenic Shock Causes, Stages, and Treatments

Cardiogenic shock is a serious condition that can result in death if medical attention is not sought out quickly. This condition occurs when the heart is no longer able to pump enough blood to meet the needs of your body. When there is not enough blood and oxygen making their way to the organs, it can result in organ failure and eventually death if not treated right away.
This medical issue is more common than a lot of people might imagine. Annually in the United States, there are around 50,000 people who suffer from cardiogenic shock. This is the leading cause of death in people who have a heart attack.
Cardiogenic Shock Causes
Even though it’s the top cause of death in people who have a heart attack, and it is the most common cause of cardiogenic shock, having a heart attack does not always lead to cardiogenic shock.
When someone has a severe heart attack, they may suffer damage to the left ventricle, which is the main pumping chamber for the heart. If this happens, it hampers the body’s ability to pump blood. The left ventricle is often the one that receives the most damage and causes cardiogenic shock. However, it could also happen to the right ventricle.
In addition to heart attacks, you will find other potential causes of cardiogenic shock. There could be inflammation in the heart muscle or an infection in the heart. Those who suffer from an abnormal heart rhythm are at a higher risk of having cardiogenic shock, as well.
Having too much blood around the heart, blood clots, or tears in the valves of the heart could lead to cardiogenic shock, too. Even if someone is considered healthy and has a good heart, an injury to the chest could damage the heart and lead to cardiogenic shock.
Types of Cardiogenic Shock: The Stages
Cardiogenic shock has several stages. The amount of time that each stage lasts can vary from one patient to the next, of course. Additionally, medical attention at earlier stages can sometimes help to curb the problem before it becomes worse.
Some people may have heart disease and other cardiac issues. This might include suffering a heart attack or heart failure but not having signs of cardiogenic shock. These issues don’t always lead to shock.
Those who don’t take steps to reduce their risk at this point may then proceed to what most consider the first stage of cardiogenic shock. This is where they have a lowered blood pressure or heart rate. Essentially, they aren’t pumping enough blood to the organs.
The next stage is when the patient starts to need medicine or medical devices that can help them get blood to their organs.
The following stage is entered if a patient is not responding to those devices or medicine, and they continue to get worse. The patient could then progress to a stage where they enter cardiac arrest and need CPR, a ventilator, or a defibrillator. At this point, it can be difficult for the patient to survive.
Ideally, patients will start to notice that they have issues with their heart as early as possible, so it never progresses beyond those initial stages. However, that’s not often the case.
What Treatments Will the Doctors Perform?
Diagnosis of Cardiogenic Shock and Emergency Treatment
First, the doctors will need to determine whether the patient has cardiogenic shock or another health issue. There are multiple tests, including lab tests, that doctors can use to provide a proper diagnosis. The treatment will depend on a range of factors including the stage of shock.
The goal is always to ensure that you have enough blood flowing from and to your heart and organs to remain healthy. This might require the use of medications, often provided by IV in cases of emergency. The patient might also have to go on oxygen to increase the amount of O2 in their blood.
Additional Treatment
After emergency medical treatment has been provided, there will likely need to be additional treatment. Again, this will vary based on the cause of the cardiogenic shock. In some cases, it might result in stent placement, heart valve repair, or a bypass. Those who have fluid around the heart will need to have it removed via a needle. This stops the compression of the heart.
Each case is different. Patients and their loved ones will want to speak with the doctors about the available options. Those who feel they may be in danger of suffering cardiogenic shock should start finding ways to reduce that risk. Talk with a doctor about medications to take and lifestyle changes to make.
Cardiovascular Research and Training Institute (CVRTI)
Researchers at the CVRTI use a multidisciplinary approach to study every aspect of cardiogenic shock from the cell to the bedside. We have Investigators who study the cell response to lack of oxygen (Chaudhuri, Hoareau, Lesniewski, Palatinus, Selzmen) and ways to preserve heart tissue when blood flow is compromised in cardiogenic shock. Individual cells are injured when blood flow is lost and receive additional injury when blood flow is restored (termed reperfusion injury) (Hoareau, Shaw). Keeping individual cells alive in the setting of shock is critical to patient survival. On the other end of the spectrum, our investigators study methods of maintaining the normal heart rhythm as abnormal heart rhythms a can contribute to cardiogenic shock (Aromolaran, Dosdall, MacLeod, Ranjan, Shaw, Tristani). Our investigators have access to heart tissue from patients who have received heart transplants for cardiogenic shock to study changes in proteins and molecular signals in response to this condition (Drakos, Hong, Shaw).


 The Drakos Laboratory, headed by Stavros Drakos, MD, PhD, focuses on understanding the metabolic and molecular profile of the failing and recovered heart and utilizes biological information derived from studies in humans, small, and large animal HF models to understand, predict and manipulate myocardial recovery. Original work generated by the Drakos research team in the laboratory and in the clinical arena led to the founding and establishment of the award winning multidisciplinary Utah Cardiac Recovery Program (UCAR). Link to lab summary page on CVRTI
The Drakos Laboratory, headed by Stavros Drakos, MD, PhD, focuses on understanding the metabolic and molecular profile of the failing and recovered heart and utilizes biological information derived from studies in humans, small, and large animal HF models to understand, predict and manipulate myocardial recovery. Original work generated by the Drakos research team in the laboratory and in the clinical arena led to the founding and establishment of the award winning multidisciplinary Utah Cardiac Recovery Program (UCAR). Link to lab summary page on CVRTI 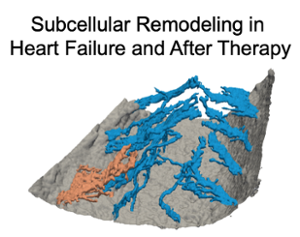 The Sachse Laboratory, headed by Frank Sachse, PhD, provides insights into structural and functional remodeling in diseased hearts and mechanisms of cardiac recovery after clinical therapy. They also develop optical approaches to support pediatric heart surgery and interventional cardiology.
The Sachse Laboratory, headed by Frank Sachse, PhD, provides insights into structural and functional remodeling in diseased hearts and mechanisms of cardiac recovery after clinical therapy. They also develop optical approaches to support pediatric heart surgery and interventional cardiology.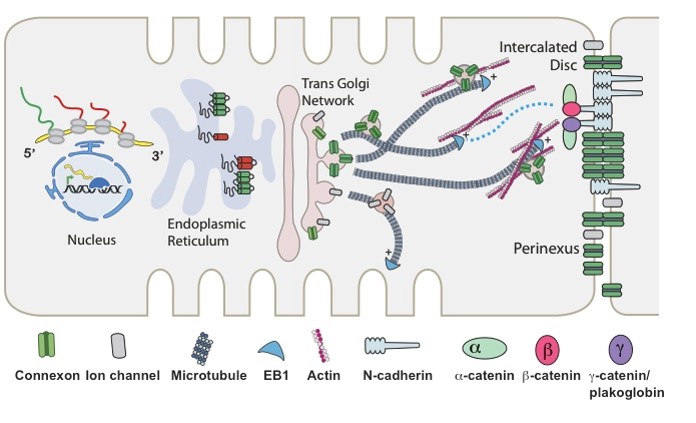 The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI
The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI The Shaw Laboratory, headed by Robin Shaw, MD, PhD, is focused on understanding the cell biology of heart arrhythmias and heart failure progression. Link to lab summary page on CVRTI 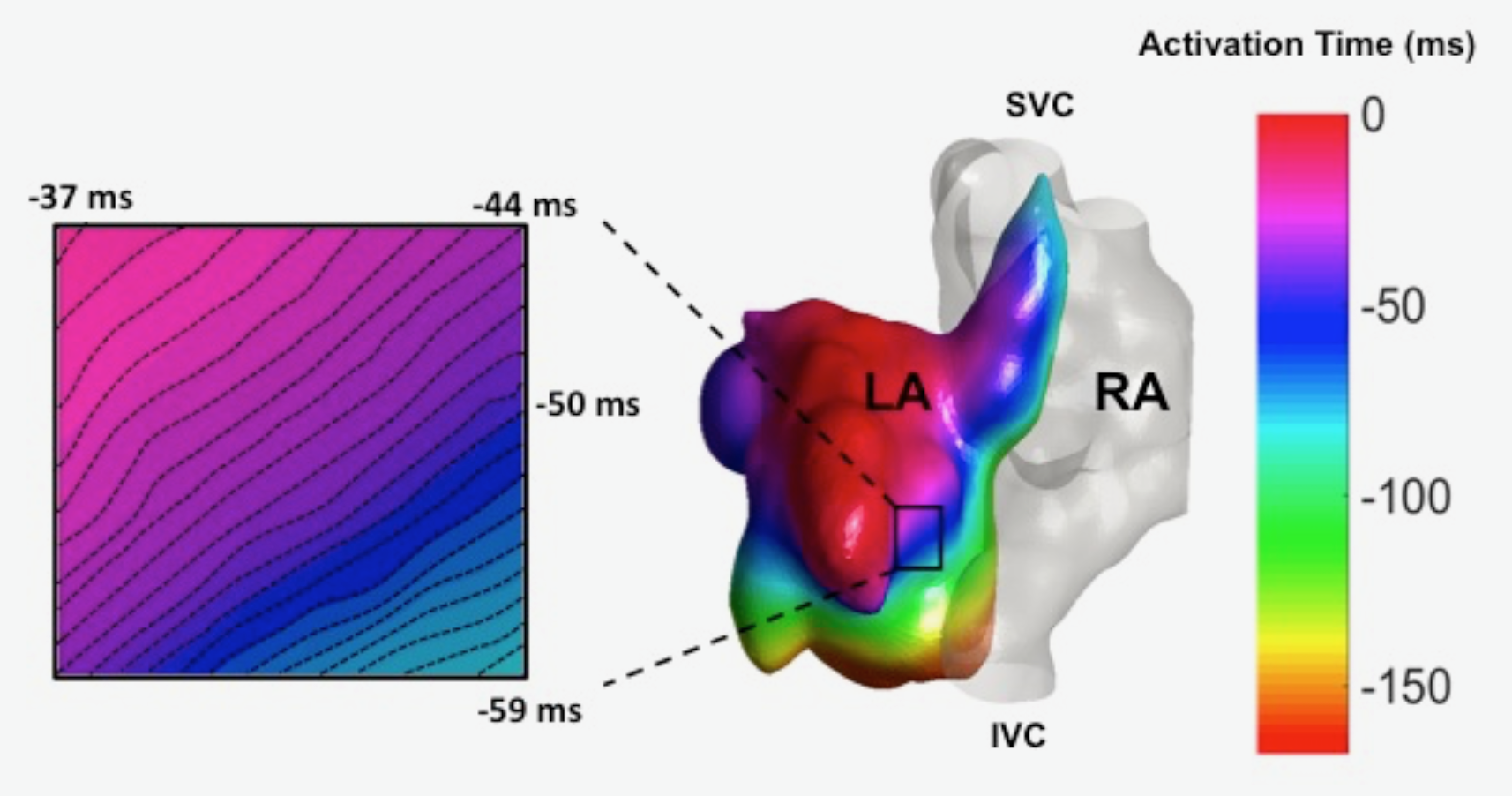 The Ranjan Laboratory, headed by Ravi Ranjan, MD, PhD, focuses on developing a better understanding of arrhythmia mechanisms and optimizing the ablation procedure. The lab is using a combination of high density electrical mapping and imaging in an animal model combined with computational modeling to develop a better understanding of arrhythmia mechanisms. To optimize the ablation procedure, the team uses MRI to quantify tissue changes including reversible edema over time for different energy sources and ablation parameters to develop the optimal ablation technique. Link to lab summary page on CVRTI
The Ranjan Laboratory, headed by Ravi Ranjan, MD, PhD, focuses on developing a better understanding of arrhythmia mechanisms and optimizing the ablation procedure. The lab is using a combination of high density electrical mapping and imaging in an animal model combined with computational modeling to develop a better understanding of arrhythmia mechanisms. To optimize the ablation procedure, the team uses MRI to quantify tissue changes including reversible edema over time for different energy sources and ablation parameters to develop the optimal ablation technique. Link to lab summary page on CVRTI 
