Heart Failure Symptoms, Early Signs, and Stages of Progression
The term “heart failure” may sound as though your heart completely stopped working, but that’s not the case. Heart failure means that the heart is no longer capable of pumping blood as well as it should be. It is a serious long-term condition that worsens over time. When the heart doesn’t pump blood properly, your organs will not be getting the blood needed to perform.
The Early Warning Signs and Symptoms of Heart Failure
Signs and symptoms of heart failure vary in type and severity. Some of the common signs include shortness of breath, swelling in the legs, ankles, and abdomen, and feelings of fatigue when you are active.
Shortness of breath can manifest in different ways depending on the severity of your condition. You may notice it’s worse when lying flat (called orthopnea), requiring you to prop yourself up with pillows to sleep comfortably.
Some people experience paroxysmal nocturnal dyspnea, where they wake up suddenly during the night gasping for air and need to sit up or stand to breathe easier.
Some patients experience persistent cough or wheezing that doesn’t go away, sometimes producing white or pink-tinged mucus. You may also notice your heart beating faster or irregularly (palpitations) as it tries to compensate for its reduced pumping ability.
Some also need to get up more and urinate during the night. They may have irregular heartbeats or a dry, hacking cough. Weight gain can occur, as well.
Sometimes the heart failure symptoms are mild or they could vanish entirely. It is important to note that this doesn’t mean that you no longer have heart failure. They may vanish for a time and then return.
Why Symptoms Occur
Understanding why heart failure causes these specific symptoms can help you recognize them early and take appropriate action. When your heart’s pumping efficiency decreases, it can’t meet your body’s demand for oxygen-rich blood, leading to a cascade of effects throughout your body.
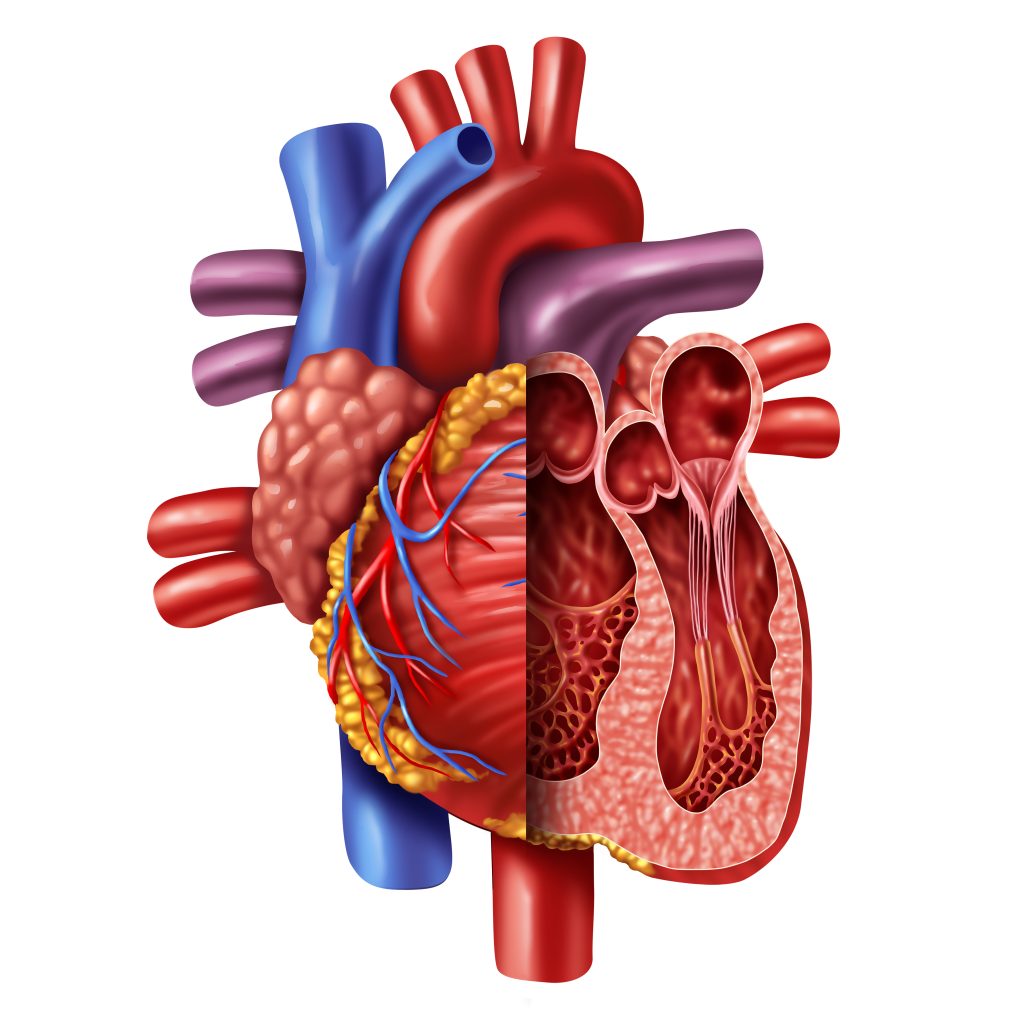
The primary mechanism behind many heart failure symptoms is blood backup. When the left side of your heart can’t pump blood effectively to your body, blood backs up into your lungs, causing pulmonary congestion. This congestion leads to shortness of breath, especially when lying down, and can cause the persistent cough or wheezing many people experience.
When the right side of your heart struggles to pump blood to your lungs, blood backs up in the veins returning blood from your body to your heart. This backup causes systemic congestion, resulting in the swelling you may notice in your legs, ankles, feet, and sometimes your abdomen.
Fatigue and weakness occur because your muscles and organs aren’t receiving enough oxygen-rich blood to function optimally. Your body may even redirect blood away from less vital organs, like your digestive system, to prioritize your heart and brain. This can contribute to feelings of tiredness and may cause loss of appetite or nausea.
In some cases, reduced blood flow to the brain can cause difficulty concentrating, memory problems, or confusion. While chest pain isn’t always present, it can occur if your heart failure is caused by an underlying condition like a heart attack.
For most patients, heart failure will continue to worsen. After a diagnosis, make your doctor aware of any changes to your symptoms.
How Is Heart Failure Diagnosed?
Your doctor will need to know more regarding your medical history, as well as your heart failure symptoms. They may ask whether you have a family history of heart disease or sudden death, whether you smoke or use tobacco, and how much alcohol you drink. They will also want to know what medications you are taking.
They need to know about other health conditions you may have, such as kidney disease, diabetes, high blood pressure, high cholesterol, coronary artery disease, or other heart issues.
The doctor will provide a physical exam to look for early signs of heart failure or other diseases that could have affected your heart muscle. They will often check your ejection fraction, which will let them know how well your ventricles are pumping blood. This can be done relatively easily with noninvasive tests. Normal left ventricular EF is between 53% and 70%.
Other tests that will determine the severity of your heart failure and its cause include various blood tests, cardiac catheterization, chest x-rays, ECGs, MRIs, EKGs, echocardiograms, stress tests, and MUGA scans.
Once the doctor determines the type of heart failure you have and the cause, they can begin treatment. The types of treatment often vary based on the stage.
The Stages of Heart Failure
Below are the stages of heart failure, along with potential treatments used at each stage.
Heart Failure Stage A
When you are at risk but haven’t suffered heart failure yet, you are considered in Stage A. Those who are at this stage can undergo a treatment plan that can help them to reduce their risk of further damage. This includes becoming more active and getting regular exercise, stopping the use of tobacco products, getting treatment for high blood pressure and high cholesterol, and not drinking or using recreational drugs.
Doctors may prescribe angiotensin-converting enzyme inhibitors or an angiotensin II receptor blocker for those who have high blood pressure, diabetes, coronary artery disease, or other cardiac issues. Beta-blockers might also be prescribed for those with high blood pressure.
Heart Failure Stage B
This is also considered pre-heart failure. The doctor has found that you have systolic left ventricular dysfunction, although you don’t have symptoms of heart failure.
In addition to the Stage A treatments, the doctor might also prescribe an aldosterone antagonist if you have diabetes or have had a heart attack and have an ejection fraction of 35% or less. In some cases, surgery may be required.
Heart Failure Stage C
Those with Stage C heart failure currently or previously had some or all of the signs and symptoms mentioned above. The Stage A and B treatments are still employed along with medications that can slow the heart rate if it’s above 70 bpm and the heart failure symptoms remain.
If Heart Failure Symptoms Continue
Diuretic pills may be used if heart failure symptoms continue, and sodium will be restricted. At this stage, patients must track their weight daily and let the doctor know if there is a change of more than four pounds. Fluid restriction could be required in some patients. The use of a biventricular pacemaker could also be required as a means of cardiac resynchronization therapy.
Heart Failure Stage D
At this point, the patient has advanced heart failure symptoms that will not get better with treatment. It is the final stage of heart failure. At this point, in addition to the treatments used for the earlier stages, more advanced treatments are needed. This may include ventricular assist devices, a heart transplant, heart surgery, or hospice care.
Patient outcomes will vary. Those who have heart failure or who are worried they are at risk should speak with their doctor as soon as possible. Getting a diagnosis and treatment as early as possible can make a difference.
Cardiovascular Research and Training Institute
Researchers at the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI) are studying what causes heart muscle to fail and are developing therapeutic strategies to both stop heart failure progression and recover failing hearts.
CVRTI Investigators are experts in muscle gene regulation (Franklin), muscle metabolism (Chaudhuri, Drakos), muscle architecture (Hong, Shaw), and treating failing heart muscle (Selzman, Drakos, Dosdall, Hong, Shaw). One therapeutic program involves using surgically implanted left ventricular assist devices (LVADs) to recover failing hearts (Selzman, Drakos).
Another involves a promising CVRTI generated gene therapy that rescues failing heart muscle, reveres the damage heart failure does to heart muscle, and improves mortality from heart failure (Dosdall, Hong, Shaw). The therapy is known as cBIN1 gene therapy and is being advanced to clinical trials.
Frequently Asked Questions About Heart Failure Symptoms
What Should I Do If I Notice Sudden Weight Gain?
If you gain 2-3 pounds in one day or 5 pounds in a week, contact your doctor immediately as they may need to make changes to your medications. Keep checking it every day, around the same time of day and in similar clothes for consistency.
Can Heart Failure Cause Confusion or Memory Problems?
Yes, reduced blood flow to the brain can impair cognitive function, leading to difficulty concentrating, memory problems, or confusion. This is more common in advanced heart failure and may be more noticeable to family members than to the patient themselves. If you or loved ones notice cognitive changes, discuss this with your healthcare team.
When Should I Be Concerned About Chest Pain With Heart Failure?
While chest pain isn’t always present with heart failure, it can occur, especially if your heart failure is caused by coronary artery disease. Seek immediate medical attention for new, severe, or worsening chest pain, especially if accompanied by shortness of breath, sweating, nausea, or pain radiating to your arm or jaw. These could indicate a heart attack, which requires emergency treatment.


