The Science of Myocardial Recovery and The Healing Process After Heart Attack
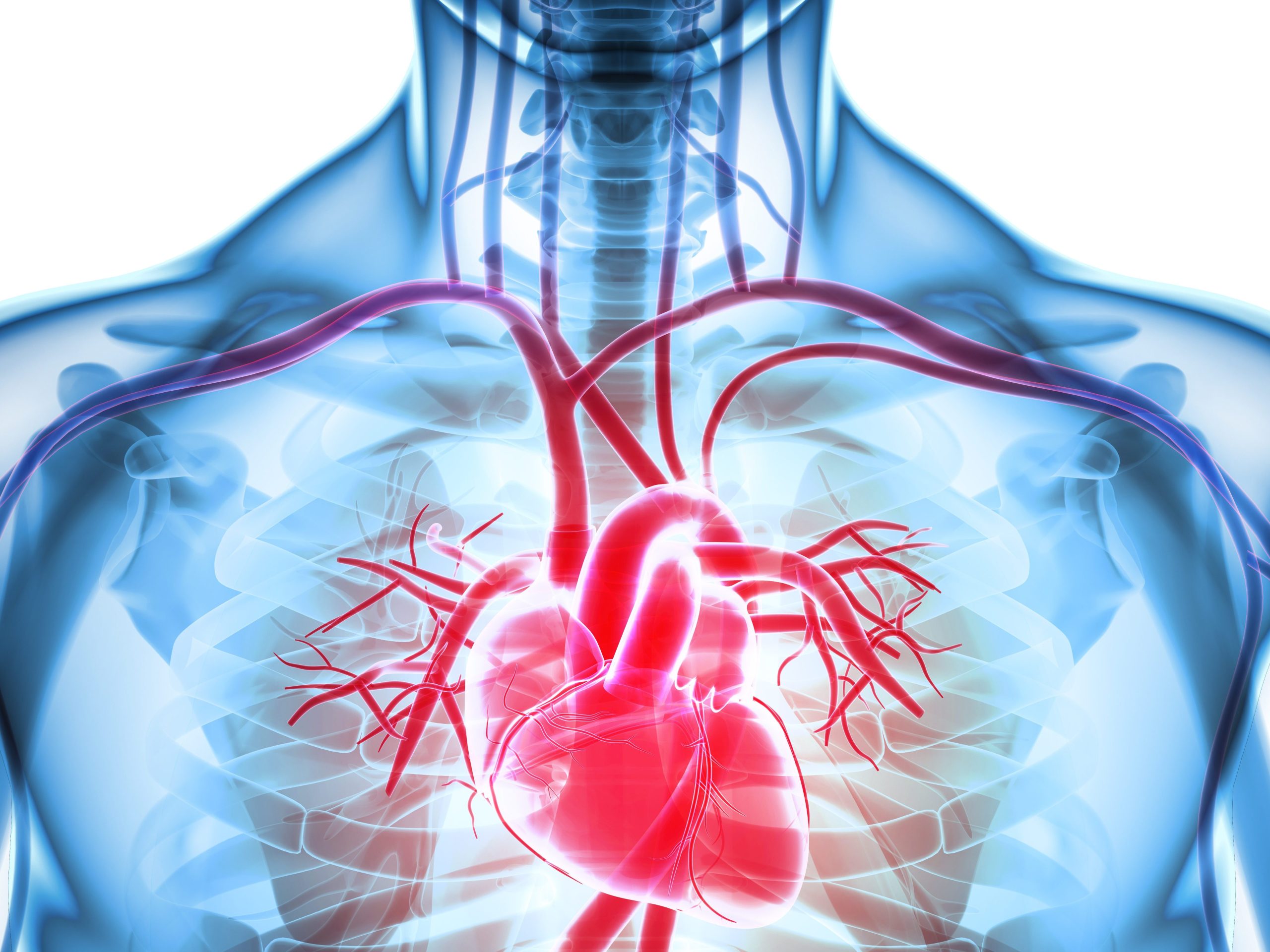
Myocardial infarction, better known as heart attack, is one of the leading causes of death in the United States. According to the CDC, around 805,000 people have a heart attack every single year, which equates to one every 40 seconds. In one-fifth of the cases, the heart attack is silent, and while the heart is damaged, the individual is not even aware of it.
The good news is that myocardial recovery – healing the heart after an attack – is possible. However, it’s important to understand the process, as well as the stages leading up to a heart attack.
What Are the 4 Stages of Myocardial Infarction?
The need for myocardial recovery is based on having a heart attack in the first place. In most cases, that stems from damage caused by myocardial infarction (the attack). While most people are familiar with the Hollywood depiction of a heart attack, the truth is that they do not always occur quickly, acutely, or painfully.
The four stages of myocardial infarction are as follows:
1. Fixed Coronary Stenosis
Stenosis is a narrowing or constricting of a passageway; in this case, it refers to a fixed narrowing of a coronary artery.
2. Acute Plaque Change
Plaques lining the artery change, either through rupturing or hemorrhaging.
3. Coronary Artery Thrombosis
This is the development of a blood clot that cuts off some or all the blood flow to the heart.
4. Vasoconstriction
This is a construction of blood vessels that increases blood pressure by slowing or blocking the flow of blood.
Of course, heart attacks are not the only things that can damage the heart and lead to a need for myocardial recovery. Myocarditis can also damage the heart muscle.
What Is Myocarditis?
Technically, myocarditis is an inflammation of the heart muscle, specifically the middle layer of the heart wall, called the myocardium. It’s usually caused by a virus but can also be caused by inflammatory conditions.
When inflamed, the heart cannot pump blood efficiently. The condition can also cause other symptoms, including arrhythmias (irregular heartbeat), chest pain, and shortness of breath.
Can the heart repair itself after myocarditis? Yes, myocardial recovery is possible. In many cases, myocarditis is self-resolving, according to Johns Hopkins Medicine. Some patients will require treatment and will not resolve for several months. Severe cases can lead to scarring, which forces the heart to work harder to pump blood and oxygen.
What Are the Stages of Myocardial Infarction Healing?
Myocardial recovery after an infarction usually follows specific stages, although they tend to overlap one another.
1. Inflammatory Response – Initially, the body creates inflammation as a defense response.
2. Proliferative Phase – During the proliferative phase, chemokines control various cell types, including reparative macrophages that help reduce inflammation.
3. Healing Phase – The healing phase involves the formation of scar tissue.
Overall, healing from a heart attack can take as little as two weeks or as long as three months, depending on the severity of the damage. However, there are things you can do to help increase your body’s ability to heal itself and reduce the risk of having another heart attack (30% of heart attacks every year are second heart attacks).
Note that if you’ve had a heart attack, you are 20% more likely to have another one within five years than someone who has never had a heart attack.
Important Lifestyle Changes for Myocardial Recovery and Risk Reduction
If you’ve suffered a heart attack, you’ll notice during recovery that your body may not behave as before. You may not be able to sustain the same physical activity level, engage in the same exercises, and even have difficulty controlling your emotions.
Activity Levels
Try to follow a gradual return to your normal lifestyle and activities that balances rest and recovery with getting up and active. Your doctor will help guide you here.
Exercise
Exercise is one of the most important preventative measures against heart attacks, but it also plays a central role in your recovery and reducing the risk of a second heart attack. A cardiac rehabilitation program can help with your initial heart attack recovery, but you’ll need to make time for exercise each day once the program ends.
Heart Healthy Diet
You’ll need to follow a heart-healthy diet for myocardial recovery. A healthy diet for your heart should include reducing the amount of saturated fat, sodium, and sugar you consume. Avoid red meat, highly processed meats (bacon and deli meat, for instance), and refined grains (white flour, etc.).
Heart Attack Recovery Conclusion
Myocardial recovery after a heart attack is possible. Many people go on to live long, full lives. However, you must get adequate exercise and follow a healthy diet, along with quitting smoking and limiting (or eliminating) alcohol.
Cardiac Recovery Research at the CVRTI
The Drakos Lab
Several different labs at the Nora Eccles Harrison Cardiovascular Research and Training Institute are very interested in studying myocardial recovery from HF. First, the Drakos lab and clinical research team has identified molecular, cellular, and physiologic features that influence myocardial recovery after circulatory support with assist devices which has altered paradigms in the field and has generated new therapeutic approaches.
Following a bedside to bench and back approach Dr. Drakos’ research team has been using myocardial tissue findings from cardiac recovery patients to guide their basic science investigations to inhibit or overactivate these specific targets using small and large animal models.
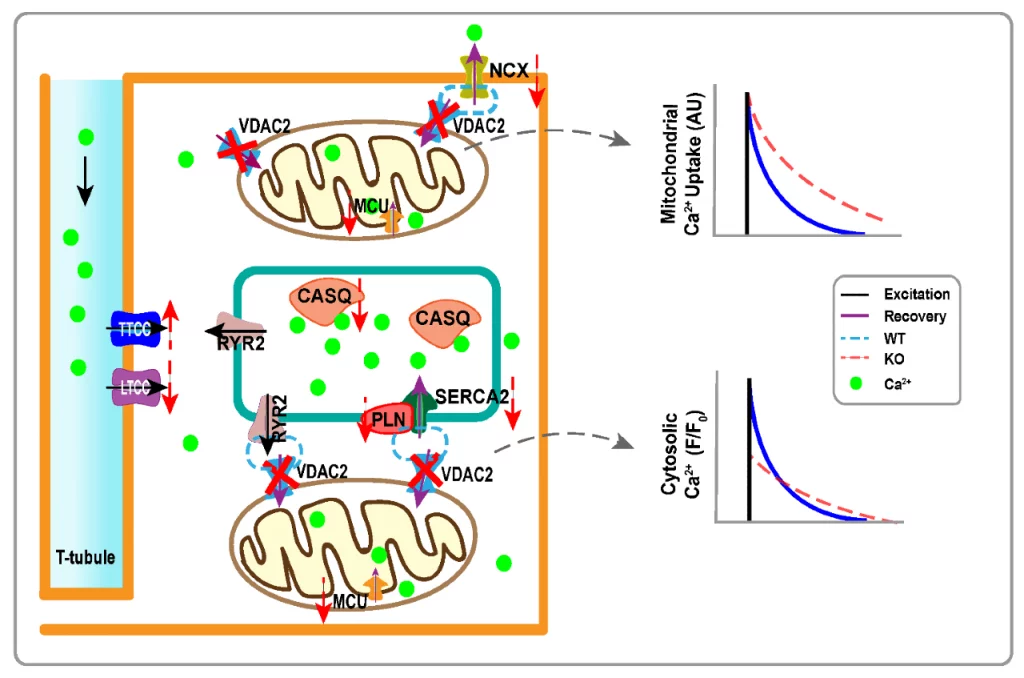
With this specific approach Dr Drakos’ research identified novel therapeutic targets for myocardial recovery: (a) MCT4 inhibition, (b) VDAC2 activation and (c) AEBP1 inhibition. Next, the Selzman lab is interested in developing “real-world” therapies to be able to help the heart recover following injury. They have very interesting data to suggest that the use of amniotic fluid (“Mother Nature’s Cocktail)” is beneficial to the heart muscle after injury.
The Shaw Lab
The Shaw lab has been working on defining the paradigm of Targeted Delivery which describes how the cytoskeleton delivers membrane proteins directly to their functional membrane subdomain and why there is less delivery in failing hearts.
In the process, the Lab discovered and named a new protein: cBIN1. This protein has a fundamental role in organizing the internal architecture of heart muscle cells and has important translational implications in the treatment of chronic heart failure to achieve myocardial recovery (cBIN1).
The Shaw and Hong Labs
The Shaw and Hong labs have together developed a gene therapy for cBIN1 that may prove extremely favorable to HF patients.
Furthermore, in the clinical research arena Drs. Drakos, Selzman and others have led in the field of myocardial recovery several studies. They published structure-function studies characterizing in detail the impact of mechanical unloading on reverse cardiac remodeling.
Furthermore, they identified practical clinical predictors, including left ventricular torsion, circulating TNFα and IFNγ and myocardial microstructural changes, that effectively guide heart failure patient selection prior to guide the most appropriate therapeutic interventions.
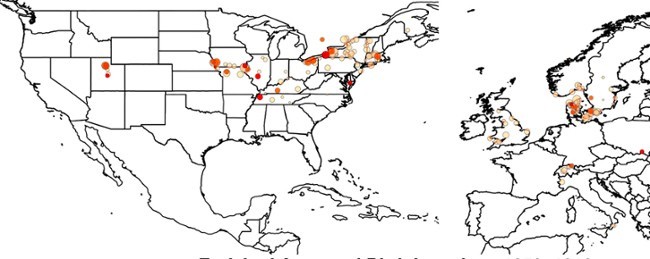
Altogether, this body of work led to the establishment of the award-winning Utah Cardiac Recovery Program (UCAR) which is currently considered one of the leading programs in the field nationally and internationally.
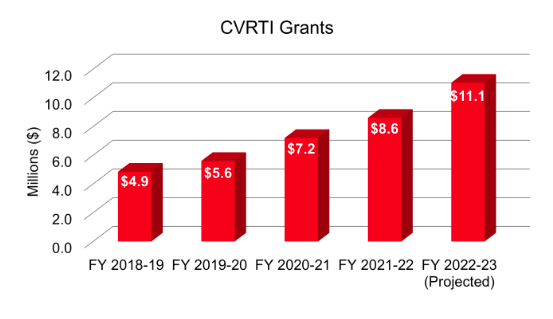
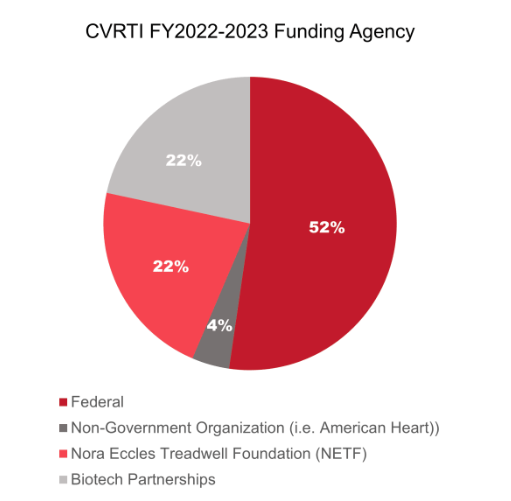
The cutting-edge research that is conducted at the CVRTI surrounding myocardial recovery and cardiac muscle regeneration will pave the way for future therapies to reduce mortality rates and improve the quality of life for the greater HF community.