Understanding the Basics of Arterial Plaque Buildup
What is Arterial Plaque Build Up?
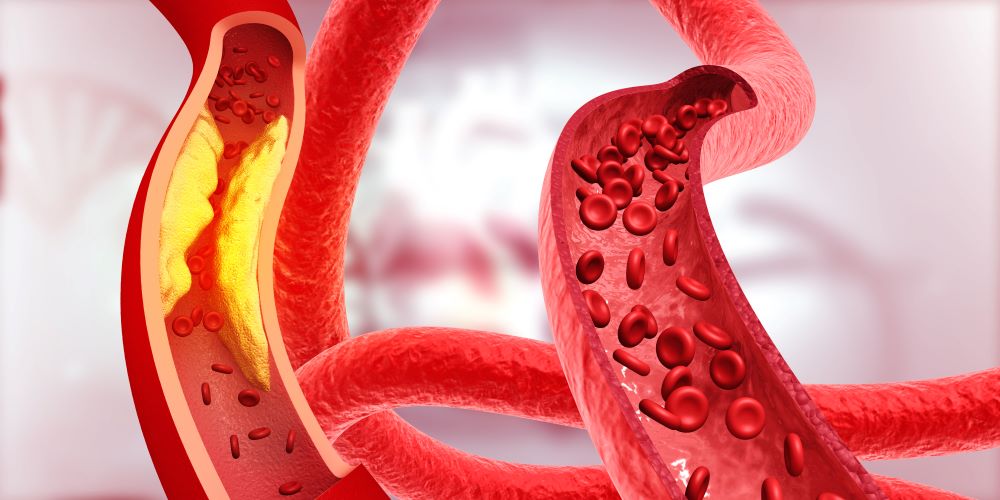
Arterial plaque buildup, also known as atherosclerosis, occurs when fats, cholesterol, and calcium deposits stick to and build up on the inner walls of arteries, potentially blocking blood flow over time. Buildup leads to a narrowing of the arteries, and the signs of atherosclerosis depend upon the severity of arterial plaque buildup and where the buildup occurs in the body.
Symptoms of Plaque Buildup and Disease in the Heart and Brain
For example, severe plaque in heart arteries could lead to chest pains and intense pressure, mimicking the symptoms of a heart attack. Sudden numbness or weakness in arms and legs, difficulty speaking, and loss of vision could mean blockages in brain arteries, mimicking the signs of a stroke or transient ischemic attack.
Symptoms of Arterial Plaque Buildup in Limbs and Organs
Buildups that block blood flow in the arteries of arms and legs will cause decreased blood pressure to limbs, resulting in extreme, targeted pain or complete numbness. If the same kind of buildup occurs in kidney arteries, the biggest warning sign will be high blood pressure, often followed by symptoms of kidney failure, frequent urination, fatigue, anemia, and blood in the urine.
Managing and Treating Arterial Plaque Buildup
Arterial plaque buildup is a serious condition that affects most people at some point in their lives. Most cases are mild and easily managed with lifestyle changes, such as healthy, nutritious diets, regular exercise, and management of pre-existing conditions, like diabetes and blood pressure problems. Severe cases of atherosclerosis can result in heart attacks, strokes, and fatalities, so consultation with a healthcare provider and early diagnosis are imperative to proper, successful treatment.
What Will Dissolve Plaque in Arteries?
Unfortunately, complete dissolution of arterial plaque buildup isn’t possible, but there are methods to shrinking and stabilizing buildups to ensure a healthier, happier life.
Lifestyle Changes to Prevent Atherosclerosis
- Nutritious, wholesome diets emphasizing healthy fats, like avocados and olive oils in moderation, can reduce the risks of atherosclerosis. Consume foods like fresh fruits and vegetables, nuts, and fish while limiting processed or red meats and foods with saturated fats. Whole grains, beans, and foods rich in fiber can also help!
- Burn body fat and get in shape with a regular exercise routine that strengthens your heart and pumps blood through your body to get your arteries flowing. Aerobic exercises can lower blood pressure and regulate blood sugar levels, making it easier to maintain a healthier body weight to avoid arterial plaque buildup.
- Avoid bad habits like smoking and drinking. Both can damage arterial linings, making you more susceptible to plaque damage.
In serious cases of arterial plaque buildup, some doctors prescribe medication, like statins, to lower LDL (bad) cholesterol and prevent further buildup. Regular blood tests can help you keep track of your LDL levels since high levels contribute to plaque formation.
What is the Main Cause of Plaque Buildup in Arteries?
Eating one cheeseburger isn’t going to suddenly block your arteries, but eating a cheeseburger three times a day for years will contribute to arterial plaque buildup. Red meats and processed foods are rich in saturated fats, which are bad for your arteries because they raise cholesterol. This triggers an accumulation of plaque on arterial walls, resulting in inflammation that narrows the arteries and blocks proper blood flow. Enough of a blockage can be fatal.
Other Causes of Plaque Buildup Include:
- Being overweight. Most overweight people have high levels of LDL cholesterol, raising their risk of heart disease and leading to arterial plaque formation.
- Age. As people age, cholesterol levels become more difficult to control. For women, LDL levels can increase significantly after menopause.
- Genetics. If high cholesterol and problems with heart disease and arterial blockages run in your family, you have a higher risk of the same.
Can You Reverse Calcium Buildup in Arteries?
Complete reversal of calcium building in arteries is unlikely, but you can prevent further buildup and stabilize existing ones with a healthy lifestyle change. Maintain a healthy weight through diet and exercise, consume nutritious and wholesome foods that are low in saturated fats, and protect arterial linings by giving up bad habits like smoking or excessive drinking. You should also have regular checkups with a healthcare provider to monitor and manage arterial plaque buildup.
What are the Steps of Plaque Buildup?
Arterial plaque buildup occurs in several stages, beginning with endothelial damage, which is damage to the inner layer of your arteries. From there, cholesterol enters the damaged arteries, forming foam cells because white blood cells attempt to digest bad cholesterol.
How Arterial Plaque Leads to Inflammation and Complications
This creates inflammation, recruiting more white blood cells to the area and creating more foam cells to thicken the arterial walls. The cycle of arterial plaque buildup continues. In some cases, a fibrous cap of smooth muscle cells forms to prevent plaque from entering the bloodstream. However, if the arterial plaque buildup continues to grow, it narrows arteries, causing a rupture that leads to dangerous blood clots.