Managing Cardiac Ischemia: Treatment Options and Lifestyle Strategies
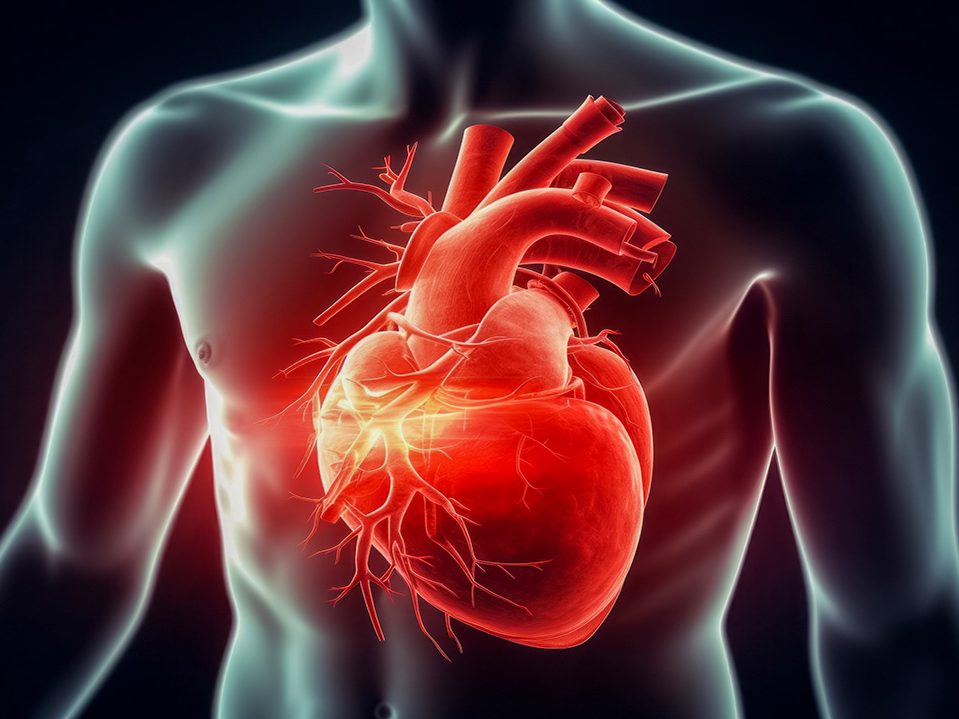
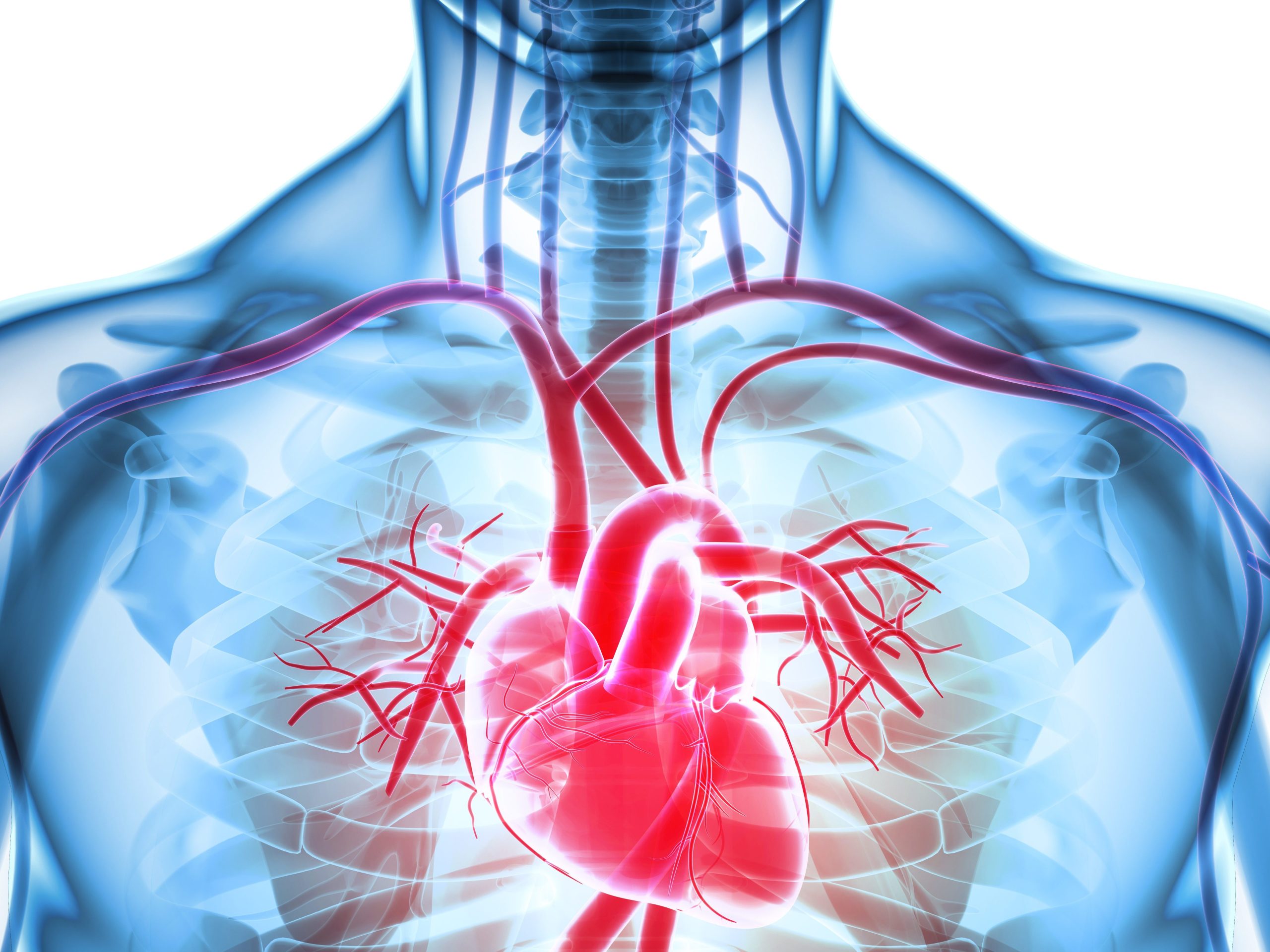
Cardiac ischemia is a condition that is caused by a loss of proper blood flow to the heart, usually as a result of buildup in coronary arteries which are the arteries that feed the heart. Understanding how to treat this condition and manage a healthy lifestyle can go a long way in making ischemia a less life-threatening diagnosis. Of course, every patient is different, so the treatment options can be different as well.
It’s important to manage this condition because ischemia can lead to a higher risk of heart attack and heart disease, as well as a higher risk of death due to heart disease or heart failure. To manage it, of course, you need to start by having a better understanding of cardiac ischemia and all that it can do.
Symptoms and Diagnosis
Cardiac ischemia is usually characterized by pain in the chest or shortness of breath when you perform any strenuous activity. It may also include arm pain, tingling or numbness, and other symptoms, but it’s generally a feeling of discomfort all around. For those with more severe cases, the pain may also be more severe and that could indicate that getting treatment is even more serious.
There are several different diagnostic tools used to determine if someone has ischemic heart disease. An EKG test can be performed while a person is resting. The most diagnostic non-invasive option is to do a stress test. This can be done with physical exercise, or for those who can’t exercise, a chemical based test can be performed instead.
In a stress test, the heart is put under a lot of exertion to see what it can handle. At the same time, you’re hooked up to an ECG and carefully monitored. There are also instances where imaging and other diagnostic tools are used alongside stress tests to get an accurate diagnosis.
Managing Cardiac Ischemia
So, how do you manage cardiac ischemia? Well, that depends on several factors. For starters, it will be important to consider how severe your condition is. Those who have milder forms of the disease may not need to do as much. A few simple lifestyle changes could make a big impact. For others, it might become a full-time job to manage this condition. As mentioned, education goes a long way in helping.
What is the first line of treatment for ischemic heart disease? Usually, it’s a combination of medication(s) and exercise along with lifestyle changes. Especially when the condition is caught early enough, these efforts can make big impacts. The changes that you make to your lifestyle and the medications that you need will depend on your specific circumstances, of course, so be sure to talk to your doctor and figure out what’s best.
Exercise and Rehabilitation
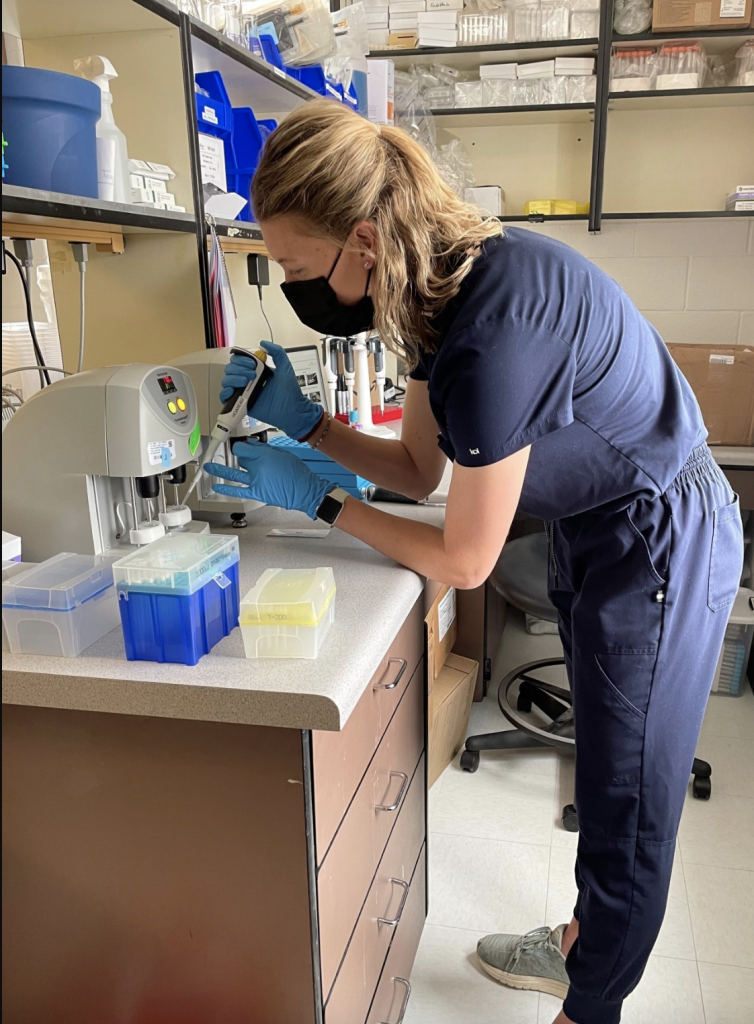
Medications can help, as do exercise and rehab. Physical exercise is best, at a level that is comfortable for the individual. This can help strengthen the heart muscle, and improve overall health.
What exercise is good for ischemia? Honestly, there’s a lot that you can do. Aerobic exercise is best, such as walking, biking, light jogging, or even swimming. If you want to stick to the gym, try an elliptical for low-impact, high-power cardio. Also, make sure that you stretch before and after you exercise to keep your muscles loose and help your heart maintain a regular rhythm.
Talk to your doctor because not all exercises are good for all patients when it comes to heart disease. Some people may be limited to light walks and water aerobics, for example, because they are easy and low impact.
Lifestyle Changes
There are also several lifestyle changes that you may have to undertake as part of managing cardiac ischemia. In addition to adding exercise to your daily routine (30-60 minutes per day, five days per week), you should also:
- Eat a diet low in saturated fats, trans fats, cholesterol, and salt.
- Eat lots of whole grains, fruits, and vegetables.
- Reduce stress and alleviate depression.
- Stop smoking.
- Limit alcohol intake (or just stop).
- Take the prescribed medications for your heart condition and other diseases.
Create Your Management Plan
The best thing that you can do if you are diagnosed with cardiac ischemia is to work with your doctor to come up with a plan to help manage your condition. This will be based on how severe your ischemia is as well as what types of rehabilitation will be most effective and will make it easier for you to take charge of your heart disease and take back your health.
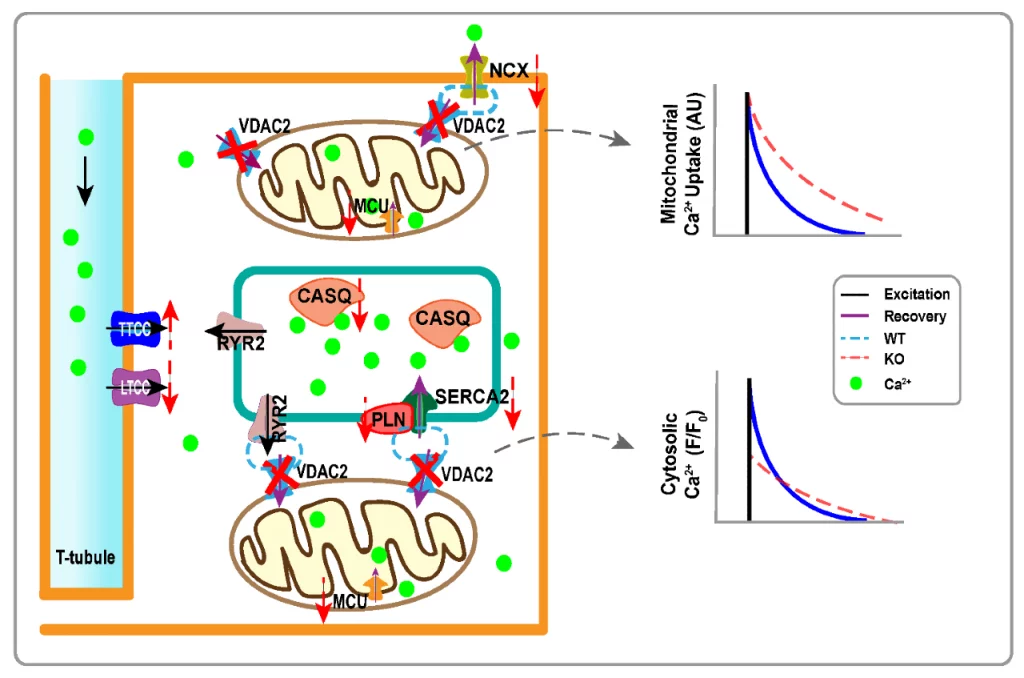
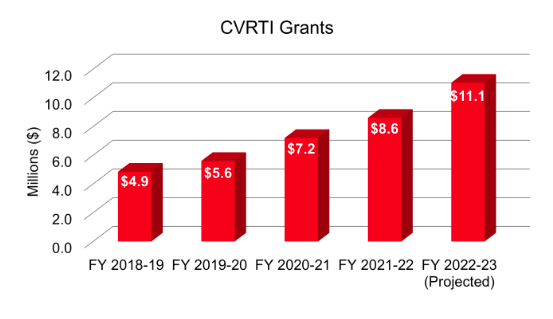
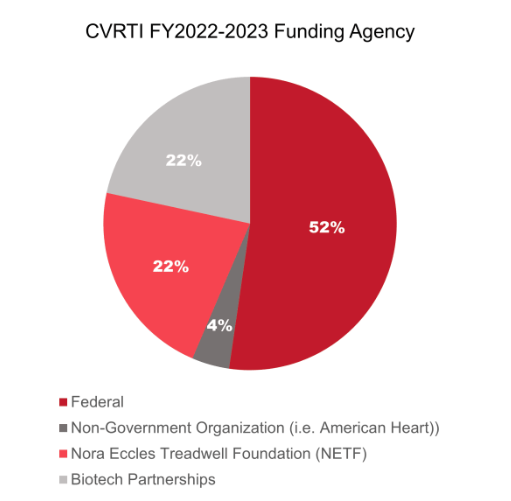
CVRTI
At the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI), many of our Investigators are working on improving diagnostics and therapeutics to better treat cardiac ischemia. The MacLeod Lab is improving EKG detection of ischemia. The Guo Lab is understanding the process of ischemia and, using stem cells, is exploring the application of anti-inflammatory agents against it. The Donato and Lesniewski Labs are experts in vascular biology and what happens with our arteries as we age. Dr. Craig Selzman is a surgeon and performs bypass and heart transplant surgeries and his lab is exploring therapeutics to lessen the effect of acute ischemia. If heart failure develops after an ischemic event, the Dosdall and Shaw Laboratories are developing therapeutics against ischemic heart failure. Collectively CVRTI Investigators understand the impact of cardiac ischemia and are leading the fight to develop new and better ways to treat it.